- There is a significant amount of detail in the review of this lecture, which goes beyond that of an entry level technologist might have to know. Therefore, please concentrate on the following:
- FDG uptake in tumor
- Compare tumor to background
- Metabolic activity of disease
- PET has several roles in oncology and you should evaluate which cancers PET FDG will image. Refer to this link to identify if this specific cancer has been approved for reimbursement. The any cancer that is FDG avid it may have one more roles
- Primary tumor to evaluation of metastatic disease
- Identifying if the patient is a surgical candidate (consider lung cancer)
- Application with patients that are on or going to be on chemotherapy
- After cancer treatment, PET used to assess reoccurrence of disease
- What types of cancer should PET-FDG be used for
- Imaging different types of cancer using PET, unless otherwise states, the radiopharmaceutical being administered is 18FDG
- Head and Neck cancers (HNC)
- Application of PET has some limited application
- Seems somewhat limited in initial staging
- These cancers arise from squamous cell (carcinoma) [SCC]
- Usually occur at the surface of the effected tissue (mucosal or epithelium)
- Will spreads downward into the surrounding tissues of the muscles, lymph nodes, and/or cartilaginous/bone
- Most common invasion is through the lymph nodes with only 10% found distally during the initial examination
- Exception to this rule is nasopharyngeal cancer that can be found in brain, liver, bone, and/or lung
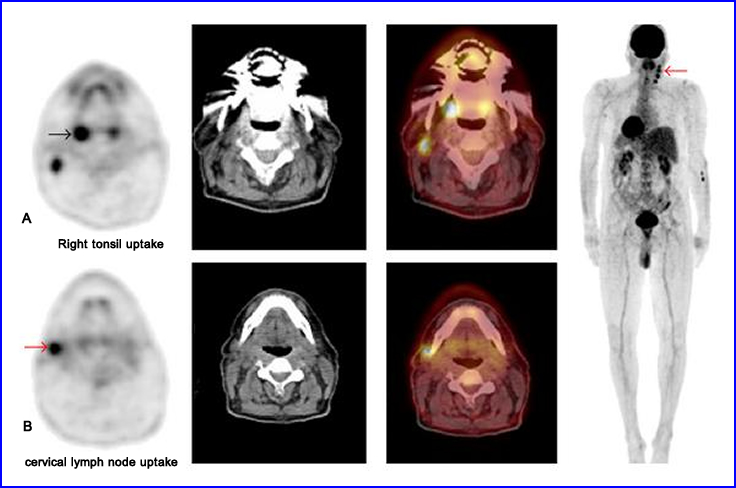
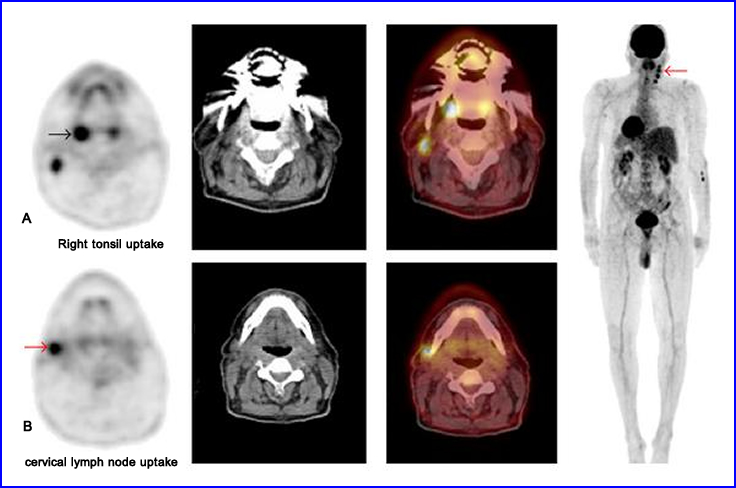
click here to see the enlarged image
- Application in the different imaging modalities
- Combining multiple studies (516 patients) CT, MRI, and PET were evaluated for the detection of lymphatic metastasis
- CT and MRI showed 59% to 86% sensitivity with 25% to 98% specificity
- PET had a 50 - 94% sensitivity and a 82% - 100% specificity
- Pitfalls
- PET may show false-positive uptake in: muscles, benign lesions, and post therapy
- CT attenuation correction may generate false-positive results when correction is applied to areas that have implanted metal, e.g. dental work
- PET should not be used in the evaluation of salivary tumors. In one example, Keyes et al identified 69% of salivary cancers with a 31% false-positive rate
- PET is recommended for the evaluation of recurrent and residue tumor
- Tagliabue et al sees little use with HNC
- Initial staging and that ranges around 12%15
- Lymph node involvement ranges between 47 to 100%
- Thyroid
- Basic review in the types of thyroid cancers
- Differentiated Thyroid Cancer (DTC)
- Papillary and Follicular Cancers (approximately 90% of all thyroid carcinomas)
- DTC is iodine avid, however, Iodine uptake is usually less than 10% when compared to normal thyroid tissue
- Distal mets may not be seen, but depends on the amount of iodine picked up by the cancerous tissue
- Following thyroid ablation, a raise in the patient's TSH level is an indication that disease is present
- 131I should be administered when the TSH level is at least 40 uU/ml
- Is FDG avid
- Medullary Thyroid Carcinoma (MTC)
- Does not pickup 131I, hence detection and treatment via this method is not suggested
- Recurrence of this disease is usually identified by measuring serum calcitonin and CEA levels
- Alternative methods of imaging are suggested
- 201Tl and 99mTc-sestamibi can be administered when the calcitonin level is at 1000 pg/ml
- Tc99m-DMSA has also been used which resembles the phosphate ion, which is taken up by the tumor
- MTC also has somatostatin sites and CEA receptors which are sensitive to 111In-somatostatin. Its sensitivity for detection is over 90%
- Is FDG avid
- Thyroid Lymphoma
- Usually appears in elderly patients with a rapidly enlarging goiter
- Patient usually has an autoimmune lymphocytic thyroiditis
- Not detected by pertechnetate or 131I
- Ultrasound, MRI, and CT may be suggested
- 201Tl, 99mTc-sestamibi, and 67Ga may be useful diagnosing this disease
- Anaplastic Carcinoma
- Usually appears as a large goiter in elderly female patient, for whom there is a poor prognosis
- The only agent that seems to pick up this type of cancer is 67Ga
- Types of thyroid cancer
- Of the types of DTC and medullary will be primarily discussed. Not as much attention will be given to thyroid lymphoma or anaplastic carcinoma, however, limited research indicates that there may be some use (ex. medullary)
- PET can be used to evaluate DTC, but is only suggested in patient that have an elevated TBG levels with a negative radio-iodine scan
- Hürthle cell (rare type of DTC) is FDG avid (example)
- PET can be used for initial staging or restaging of disease
- Evaluation of medullary cancer should be considered when calcitonin levels are elevate
- Diagnosing thyroid cancer
- The use of sonography and final needle biopsy are usually the modalities of choice
- MRI has also be used to evaluate this disease from a morphological standpoint
- CT is not recommended due to its use of radio-iodinated contrast
- Radio-iodine is recommended for staging and restaging, however, there is concern of 131I stunning that may reduce iodine uptake in cancer cells and generating false-negative data
- Thyroglobulin (TGB) is an excellent marker in patient's with a ablated thyroid, since only residual thyroid cancer will produce TGB
- PET can be used for DTC, Hürthle cell carcinoma, and medullary carcinoma. There may be some indication that anaplastic and lymphoma may have some application
- FDG-PET is 92% sensitive and 80% specific in finding Hürthle cell carcinoma (follicular cancer)
- Medullary can be diagnosed via DMSA, MIBG, MIBI, and octreotide, however, FDG seems to be the most sensitive for detection
- PET's false-positive results
- Diffuse uptake within the thyroid is usually an indication of chronic thyroiditis
- Following the injection it is imperative that the patient does not talk for the first hour! Otherwise muscle uptake will occur around the larynx and might obscure disease
- Nerve palsy caused by surgery may result in unilateral FDG uptake. If paralysis of the vocal cord occurs teflon prosthesis maybe in planted and these may cause FDG uptake which may be due to inflammation
- Possible exceptions to general belief with the detection of thyroid cancer
- Nakadte, M, et al evaluated a small group of patient to compare FDG uptake with primary thyroid lymphoma (PTL) to chronic thyroiditis. Remember, FDG will go to infection
- SUV values where higher with the PTL group (subdivided into large B-cell lymphoma and mucosa-associated lymphoid tissue) in comparison to chronic thyroiditis [25.3 to 7.4]
- In addition, B-cell had a greater SUV value when compared to thyroid lymphoma13
- Gavriel H, et al looked at accidental thyroid cancer finding when patients underwent a PET for a different reason14
- Twelve patients underwent thyroidectomy
- The breakdown from histology from surgery reviewed : 12 with papillary 5 with follicular, and 2 with medullary carcinoma
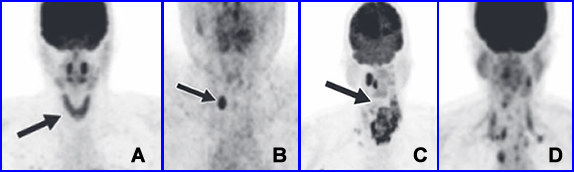
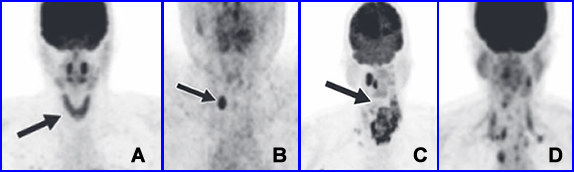
- Marcus C, et al discusses cancer management with FDG and other PET radiopharmaceuticals16
- The article reviews FDG avidity in papillary, follicular, Hurtle cell, anaplastic, and medullary cancers
- The above images from the article include: A) Thyroiditis B) Papillary, C) Anaplastic, and D) Medullary
- In this article there is also a discussion on the use of 124I, 18F-dihydrox phenylalanine, and 68Ga-adotatoc
- Esophageal, Stomach, and Large Intestine14
- Esophageal cancer (example)
- Histologically there are two types: squamous
cell carcinoma or adenocarcinoma
- Squamous shows a relationship between the presence of disease and the abuse of alcohol and/or tobacco
- Adenocarcinoma seems to be associated with gastric reflux and Barrett's esophagus
- Staging of this cancer (esophagus and gastric) is based on TNM
- T stands for depth of invasion
- N relates to the lymph node involvement
- M states the extend of distal metastatic disease
- Treatment
- Prognosis is very poor
- Surgery seems to have the best outcome, but only if the cancer is caught early
- Chemo/radiation treatment have little to no effect
- Patients in stage IV do not live beyond 5 years
- Diagnosing disease
- Gold standard is endoscopy
- PET/FDG has only shown some effectiveness with diagnosing severe dysplasia that relates to precancerous conditions ( Barrett's esophagus)
- CT is used for staging but has difficulty in determining if questionable pathology contains cancerous cells
- Laparoscopy is used routinely for evaluation of distal metastatic disease, with associated morbidity/mortality
- Recurrence of disease is evaluated via endoscopic ultrasound, and CT, but at this stage the disease is fatal
- All this said, PET does have a significant role
- Is there a role for PET?
- In locoregional disease PET has limited resolution and therefore misses small tumor/lymph nodes. However, it usually does pickup primary tumor (pending size). Flamen et al. 95% sensitive in finding primary tumor and those missed had reduced tumor size
- Luketich et al. found lymph node involvement 95% with a 45% specificity
- The issue of size may cause difficulty in distinguishing between tumor and lymphatic involvement - is it tumor or is it lymph node?
- PET has been show to be twice as accurate as CT, however, PET misses lesions smaller than 1 cm
- PET has been shown to be useful in distal metastatic disease and may prevent the use of laparoscopy
- In regards to therapy PET/FDG can help in evaluating the therapeutic process
- Tagliabue L, et al general analysis states15
- PET is effective in esophagus and stomach cancers with regards to staging and restaging
- More specific than CT and ultrasound in assessing therapy and locoregional involvement
- Can determine if surgery is an option based on the lack of lymph node involvement, however, it may miss a small volume
- False positive occurs with infections of the lower esophagus and/or questionable tumor
- False negative occurs where lymph nodes are close to the cancer and it is be seen as just a primary tumor
- Colorectal cancers
(CRC) - (example)
- Primary
disease
- Initially seventy percent of patients are candidates for resection. Of this group 30% - 40% have recurring disease
- Carcinoembryonic antigen (CEA) is used to monitor recurrence, however it is only 59% sensitivity
- For the most part CT and MRI are used to restage disease, but are limited by anatomical issues, whereas PET can evaluate the metabolism of the tissue in question
- At this time it seems that PET is not used to initially stage or screen for CRC1
- Endoscopy, barium enema, and CT colonography seem to the methods of initial discovery
- Recurrence
- While CT and MRI have issues with fibrotic tissues and scarring, FDG accuracy is 95% in the pelvis (Libutti, et. al.)
- MRI and CT accuracies are significantly lower
- Schiepers et. al. showed that hepatic metastases could be detected most accurately with FDG. Other authors had similar findings. Extra-hepatic disease showed similar results as well
- Clinical management with radiation or chemotherapy show that individuals who respond to treatment will having reduced FDG uptake
- Co-registration with PET/CT images will show a degree of mis-registration which occurs with lung/diaphragm movement is involved
| 2004 Study Combining 32 Studies |
Sensitivity |
Specificity |
| PET Extra - Hepatic Lesions |
92% |
95% |
| CT - Extra - Hepatic Lesions |
61% |
91% |
- Taglibue15 gives us the numbers above and based in the information clinical management with PET was altered ~32%
- It is further suggested that PET/CT with contrast may replace diagnostic CT per-operative staging
- PET/CT appears to be better with GI carcinoma when compared with MRI and CT. The only acceptation appears to be be small metastatic lesions in the liver, where MRI was the superior diagnostic too
- Example
- Lung Cancer
- Types of lung cancer
- Non-small cell lung carcinoma
(NSCLC) - example
- If found early, surgical resection, chemo/radiation therapy are appropriate and effective
- The problem is that when it is initially discovered it has already metastasized
- There are multiple subtypes that have varying characteristics
- Adenocarcinoma (~50% of subtype) - example
- Usually found in the peripheral lung
- In woman who are non-smokers
- Bronchiolar carcinoma [BAC] (~30% of subtype) - example
- Subtype of adenocarcinoma and grows around/within the alveolar
- Usually found as a single nodule or multiple nodules throughout the lung
- Does not grow beyond the supportive tissues (Strom) surrounding the lung
- Squamous cell carcinoma (~15% subtype) - example
- Associated with smokers, grows slowly, but rarely goes distal
- Usually a large tumor with central necrosis
- Regional node involvement can be identified
- Formation of a Pan coast tumor is typical and found in the apex of the left or right lung. See prior example with NSCLC
- Oat cell carcinoma
(~10-15%)
- Less common
- Usually found in the bronchi and grows rapidly
- Associated with smoking
- Large cell carcinoma (~5%)
- Associated with smoking
- Because this is a fast growing tumor it has already metastasized when initially diagnosed. This results in a poor patient outcome
- Small lung cell carcinoma [SCLC] (~15%)
- Patient usually does not undergo surgery, but this type of cancer responds well to chemo/radiation therapy
- Long term survival is poor
- Blithesome (MPM) - example
- Found in the pleura of the lungs and linked to patient that have been exposed to asbestos
- Metastatic disease is noted within the lung and is usually found in the in the same lung (60%) or contra-lateral side, involving the Hilary/medicinal nodes
- Detection of disease
- PET and CT
- CT is great for anatomical detail, however, abnormal lymph nodes can be either benign or malignant
- PET can determine if the area in questions has disease by the avidity of FDG. Spatial resolution for finding disease is 4 to 6 mm
- Single nodule
with 61 patients
(Gupta et al.)
- PET sensitivity was 93%
- PET specificity was 88%
- PET can also be used to identify recurrence and after radiation therapy
- SCLC
- PET can help in staging the disease
- Assess medicinal lymph node involvement
- Helps in planning radiation treatment as well as post treatment to assess the effectiveness of therapy
- MSM
- Cutoff value for SUV is 2 with higher values being associated with disease
- PET has a role in staging disease and in determining the location of MPM
- In the evaluation of 28 patients the sensitivity was 91% and specificity was 100%
- The intensity of FDG uptake helps to determining the patient's survival rates
- Evaluation lung cancer after treatment
- While CT shows great anatomical detail PET will determine if there is any functioning tumor
- Assessment with PET should be done 2 months post treatment
- False-positive results
- With carcinoid tumors and BAC
- Inflammatory disease and infections (tuberculosis, eosinophilic lung disease, histoplasmosis, and aspergillosis)
- Most chronic inflammations have low SUVs. It has also been suggested that if there is an are uptake in question, to rule of infection, rescan the area an hour later. If the SUV value drops then its infection. If the SUV goes up, it's tumor
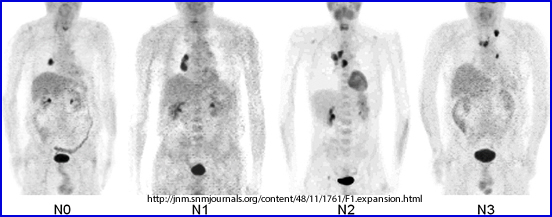
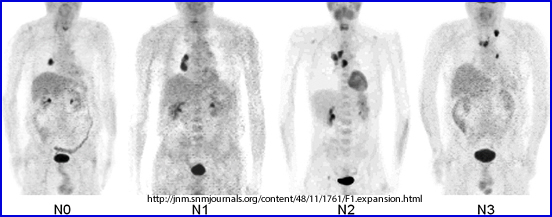
- Staging
- The above stages of lung cancer are noted
- N0 - no lymph node involvement
- N1 - Lymphatic involvement with peribroncial or hilar nodes
- N2 - Ipsilateral (same side of the body) mediastinal and subcarinal lymphs
- N3 - Contralateral and supraclavicular lymphs
- PET seems to be useful in staging MSM and NSCLC and should be done with CT
- Helps to determine the area of biopsy
- Gambhir et al. showed that when PET is used in evaluate NSCLS it helped reduce cost and predicts patient survival
- PET cannot detect lymph node involvement if the size is less than 4 - 6 mm
- Breast Cancer
- Types of Breast cancer
- Consider two aspects when defining primary breast cancer and that which goes beyond the tumor bed
- In situ is when there is only primary involvement
- Infiltrating does not goes beyond the breast tissue
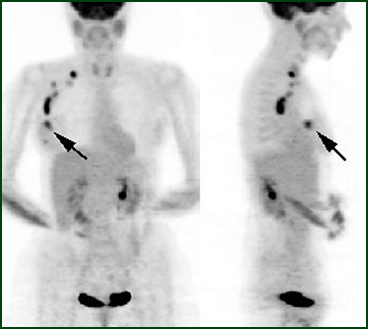
- The above image is an example of how breast cancer spreads. The arrow points to the primary tumor that negative with mammography and an Ultrasound biopsy. Above the patient's primary tumor has spread through to the axillary lymph node
- Ductal
- DCIS (In situ) - primary cancer occurs in the milk ducts
- IDC (invasive) - beyond the primary (example)
- Lobular
- LCIS (in situ) - primary cancer that occurs with the lobules
- ILC (invasive) - goes beyond primary
- Inflammatory breast cancer (IBC) - this rare form of cancer (1 - 3%) occurs in the soft tissue of the breast blocking lymph vessels causing an appearance of an infection
- Papillary - generates finger like projections (papules) as seen under a microscope. Occurs in about 3% of the population and has a better prognosis when compared to other forms of breast cancer (example)
- Triple negative breast cancer (TNBC) - has no breast receptors and occurs in about 20% of the population. Is usually invasive and originates in the ducts
- Breast cancer
uptake by PET
- There are many forms of breast cancer that have a multitude of components within the tumor cells that may or may not pickup FDG
- When compared to other cancers' SUV values, breast cancer tend to be lower
- Spread of breast cancer
- Microscopic disease is not detectable with PET's and relates to its "limited resolution"
- Primary tumors can be detected, but it depends on size. As an example, PET sensitive was 68% in tumors smaller than 2 cm
- The ability to identify regional disease or lymph node seems to have a relationship between the initial size of the tumor size and axillary node involvement
- In metastatic disease Dehdashti et al. found that sensitivity was 89% and specificity was 100 with an SUV of 2 or greater
- When comparing 99mTcMDP to FDG, FDG is the more sensitive agent for detecting bone involvement
- Schirrmeister et. al. compared Na18F in bone to 99mTcMDP and found that 18F discovered more than twice the amount of bone lesions
- Specific types of breast cancer and FDG uptake
- In-suti is the less invasive form of breast cancer because the cancer cells tend to stay local and have not yet spread. In comparison to invasive ductal carcinoma (IDC) Ruibal A et al. noted: (1) In-suti has a lower SUV value and must be at least 1 cm in size to be detected with FDG and (2) regardless of tumor size, invasive disease had higher SUV values and a greater detection rate (89%)8
- Positron Emission Mammography (PEM) evaluated different types of breast cancer: Overall invasive disease was detected 92% (33/36) [mean SUV = 2.55], invasive ductal 90% (27/30) [mean SUV = 2.62], and invasive lobular 75% (3/4) [mean SUV = 1.49]9. The FWHM of this imaging system is 1.9mm
- What is the difference between invasive ductal (IDC) and invasive lobular (ILC)? IDC forms where the ducts produce milk. It will invade surrounding tissue, stay loco/regional and go distal. ILC behaves similarly, however, its origin starts in the lobes that produce breast milk and invades other tissues. It's aggressiveness is similar to IDC
- Treatment response and re-occurrence
of disease
- If FDG uptake increased following antiestrogen therapy then the response is considered positive (metabolic reaction to therapy)
- Patients treated with only one cycle of chemotherapy that have reduced FDG uptake tend to go into remission. According to Smith el al. there is a 90% sensitivity and 74% specificity for this to occur
- In general, numerous authors concluded that if FDG uptake decreases through the course of treatment then the chemotherapy agent is effective
- One negative finding showed that after completion of therapy, if FDG was negative one could not conclude with 100% confidence that cancer was completely eliminated. The reason for this is that occult tumor may still be present
- Dedicated PET camera for breast imaging, Positron Emission Mammography
- (PEM)
- Development of a smaller PET scanner has been developed, however, results on this type of imaging system seems limited in the literature
- The reality of a smaller camera, should in theory, remove significant soft tissue attenuation and thus improve resolution

- The above system allows for breast compression, has a FWHM of 1.5 mm and has a reported sensitivity of 90% or greater
- In the above system, PEM, the image shows a lesion on the left that was not detected by mammography
- Other PET radiopharmaceuticals
- 18F-17estradiol (FES) maybe used on certain breast cancers that have a significant numbers of estrogen receptor sites. Given the right population McGuire et. al. achieved a 93% sensitivity for detection of disease
- 11C-methionine is sensitive in detection large primary breast cancers (3 cm). Uptake is caused by its association with large S-phase fraction (SPF) measured with flow cytometry. Apparently smaller tumors have lower SPF rates while larger tumors have increased SPF rates. The increased rate defines 11C-methionine uptake
- FLT may be another consideration, however, no current literature has been defined 3/15
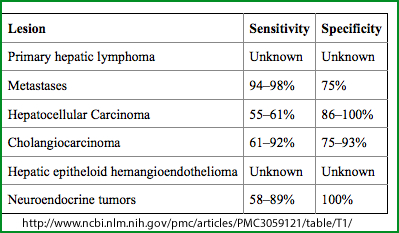
- Liver and Pancreas
- Liver
- PET (FDG) has no application in
- Detecting well-differentiated hepatocellular carcinomas (HCC) and it may the "cell differentiation" that effects FDG uptake
- Does not pickup in locoregional disease
- Following chemotherapy, FDG is secreted by the hepatic ducts which may interfere with the diagnosis of disease
- Abscesses and infections are FDG avid and may complicate the diagnosis
- Benign solid tumor
and FDG behavior
- Hemangioma - FDG shows normal or decreased uptake on delayed images
- Focal nodular hyperplasia - lack FDG uptake
- Infection/inflammation - slight to increased FDG uptake and may mislead diagnosis of colorectal cancer (CCA)16
- HCC sensitivity ranges between 38% to 70% and a specificity of 60%. Size, differentiation, and background may be factors16
- Neuroendocrine tumors within the liver and pancreas have better results with octreotide image16
- Adenomas - lack FDG uptake
- Benign cyst - lack FDG uptake
- Echinococcal cyst lacks uptake (larval stage of a tapeworm)
- Necrosis - lacks FDG uptake
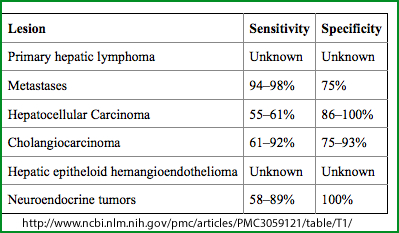 16
16
- Current literature search as of 3/15 has show some additional data with PET/FDG's ability to find cancer of the liver. Overall PET FDG is not recommended16
- PET has been used with
- Disease outside the liver were FDG is avid in metastatic disease, even in distal locations. This may have an appropriate application
- FDG has been positive with some poorly-differentiated hepatocellular carcinomas
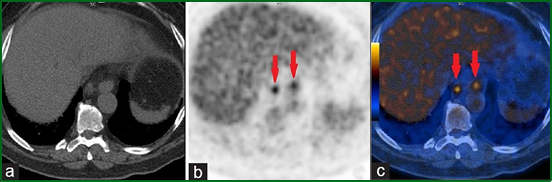
- Li J, et al. evaluated 18 people for intrahepatic cholangiocarcinoma (example) cancer and concluded: (1) sensitive in detecting lymphatic and distal disease, but limited with detecting primary tumor10
- Blechacz, et al demonstrates the use of FDG with the diagnosis of cholangiocarcinoma (example)
- There may be some application to pre/post therapy evaluation
- Pancreas (example)
- Prognosis
- Any patient that shows symptoms of this disease usually has an advanced stage of this cancer
- Surgery can have a positive outcome if pancreatic cancer has not infiltration beyond this primary area
- 37.2% of tumors <2cm already have lymph node involvement17
- Most cancers are adenocarcinomas
- Diagnostic approach
- Usually CT is used to evaluate this disease, while MRI has shown similar accuracy
- Friess et al. has shown that PET (FDG) is 94/98% sensitivity and specific in detecting disease, which is significantly better than CT (example)
- In order to differentiate between chronic inflammation and the adenocarcinomas it is suggested that dynamic and delayed images are taken. SUV values are compared. If the value goes up it's cancer, however, if the value stays the same or decreases, then it's inflammation
- Saif MW, et al. evaluated 12 patients with pancreatic cancers (2008) and concluded that PET should be used with CT, because FDG greatly improved the detection of disease. Furthermore, the improved accuracy helped physicians determine a more appropriate course of therapy action4
- Staging - While there has limited data with, CT with contrast vs PET FDG reveals that CT does a better job. It may be suggested that if PET/CT be used for staging then contrast also be applied17
- PET/CT in one study identified tumor recurrence 96% while CT and MRI 39%. However, when metastasizing to the liver CGT and MRI were superior17
- PET/MRI does show improved diagnostic accuracy over PET/CT (96.6% vs 86.6%)17
- GU
- Physiology of FDG
- Since FDG is a fake sugar it is excreted via GFR. This may present some difficulty with disease found in the GU, if urine is a background factor and presenting a possible false negative diagnosis
- Glucose follows the same pathway as FDG, however, following GFR elimination only glucose is reabsorbed by the tubules
- Renal to Bladder
- FDG is mildly picked up by renal cell carcinoma and for this reason it is not recommended for primary diagnosis
- CT, MRI, and sonography are the methods of choice for diagnosing this disease and evaluating the extent of involvement
- PET does show distal metastatic disease, however, this type of application is currently not being used in the management of this carcinoma
- Win et al states that from a 315 patient study his colleagues were 100% sensitive and 100% specific in diagnosing metastatic disease confirmed by biopsy. Restaging with FDG was also suggested
- He was unclear as to FDG application with initial diagnosis
- The author suggests when imaging the renal area the patient to should drink lots of fluids and/or be given a diuretic. This should "dilute" the FDG be excreted
- The above image shows a normal CT scan where PET FDG identifies para aortic lymph nodes containing disease
- Bladder cancer (example)
- Greater occurrence with men who smoke
- Most cancers are transitional cell carcinomas that develop from the epithelium. To a lesser degree some bladder cancers maybe of squamous or adenoma in nature
- While there maybe a role of PET with distal mets, there is no application for locoregional disease
- Adrenal cancers
- In detecting pheochromocytomas 29 patients were comparing with FDG and MIBG. PET actually found 4 additional cancers that were not seen with MIBG
- PET-FDG may be considered when MIBG is negative
- In one study of 17 patients, FDG PET was 100% sensitive and 90% specific in diagnosing adrenocortical carcinoma 18
- Adrenal cortical carcinomas PET effected the staging and cancer management of a selected group of patients indicating that PET has an application with this disease
- Genitalia
cancer
- Ovarian (example)
- This epithelial cancer is the 5th leading cancer death for woman and usually occurs with 65 years or older. Prognosis is poor since disease has already spread when at its initially diagnosis
- Cancer-associated antigen (CA 125) levels may correlate with survival and staging
- This cancer spreads into the peritoneum or paraaortic lymph nodes
- While CT and MRI are used to evaluate the peritoneum, laparoscopy, is used for staging
- PET-FDG has show some positive results in pre-laparoscopy patients and may be better than CT or MRI (One study by Hubner was positive with FDG uptake while Kubik-Huch saw no difference)
- PET does show uptake in inflammation, benign cystadenoma, endometriosis, and endometrioma
- Uterine cancer
- Cervical and endometrial cancers are the most common while uterine sarcoma are present in no more than 3% of the population (example)19
- Endometrial cancer usually occurs in postmenopausal woman and spreads through the endometrial wall into the lymph system. Dissemination into the lungs may occur
- Cervical cancers usually appear in woman that are in their mid-forties and have contracted the human papillomavirus (HPV). Routine Pap smear is suggested for early detection which usually results in the diagnosis of disease at the local level
- Transvaginal ultrasound, MRI and CT are used to diagnose these diseases however, detection in the lymph system is poor using these modalities
- PET may have some impact in lymphatic staging with paraaortic lymph node is critical in defining the spread of disease
- Vulva cancer (example stage III)
- This curable form of cancer depends on inguinal node involvement
- PET may have a role in the determination of lymphatic involvement
- Prostate cancer (example)
- Cause of this cancer is unknown
- PSA levels, CT, MRI, and sonography have been used to diagnose this disease
- PET-FDG has had little to know use while [11C]methionine has detected locoregional and distal metastatic disease, but to date this data is limited
- [11]Choline may also have some advantages in and may differentiate between benign and malignant disease by quantifying the SUV. Prostate lesion to muscle ration and prostate cancer had an SUV of 4.21 +/-1.61 while benign disease was 1.87 +/-09855
- Testicular cancer
- This germ cell cancer usually occurs in the male population between the ages of 20 - 35 years
- Two categories: seminomatous (example para-aortic nodes) and non-seminomatous (GCT) [mixed cells]
- GCT may have high levels of human chorionic gonadotropin
- These cancers respond well to chemo/radiation therapy
- CT, ultrasound, and surgery seem to main diagnostic tools with CT having a high false negative rate in staging
- Seminomas have higher levels of FDG uptake when compared to GCT
- PET vs. CT - PET 92 % to 52% in specificity of all cell types
- PET is recommended for evaluation in recurrence of all testicular cancers
- Penile cancer
- This rare form of squamous cancer can metastasize to the inguinal and pelvic lymph nodes
- There is only one study by Ravizzini et al. that identifies locoregional and distance mets with FDG
- Lymphoma (non-Hodgkin's lymphomas) ["Pictorial Essay" - article]
- Types of lymphoma - For more information of the disease types click here
- B-cell lymphoma [DLBCL] (85%) - usually occurs in an older population (~65 yrs of age). Starts as a fast growing mass in lymph nodes deep within the body. Typically seen in abdomen or chest. Easily treated with chemotherapy
- Primary mediastinal B-cell is a subtype of DLBCL . Involves about 2% of the population, most women contract it, usually around 30 or so years of age. Fast growing, underneath the mediastinum. It may effect breathing and blood flow, with has a 50% cure rate
- Intra-vascular large B-cell - Subtype DLBCL are found inside blood vessels and not in lymph nodes
- Follicular Lymphoma
- Usually grow in a circular pattern inside lymph nodes. Occurs in 20% of the population with a mean age around 60.
- Not treated until there is a problem. About a 1/3 turns into DLBCL
- Chronic lymphocytic leukemia (CLL) and small lymphocytic lymphoma (SLL)
- Similar types however, found in different areas of the body
- CLL is found in bone marrow and blood
- SLL is found in spleen and lymph nodes
- Low growing and poor outcome, however, patients can liver for over 10 years with this disease
- Mantle cell lymphoma
- Slow growing and found in about 5% of all lymphomas. Usually occurs in men around the age of 60. Initial diagnosis will find it in the spleen, lymph nodes, and bone marrow. Treatment seems to be improving with this disease
- Marginal zone B- cell lymphomas
- Makes up between 5 to 10% of lymphomas, small in size and has three subcategories: Extranodal marginal zone B-cell lymphomas, also known as mucosa-associated lymphoid tissue (MALT) lymphoma, Nodal marginal zone B-cell lymphoma, and Splenic marginal zone B-cell lymphoma
- Burkitt lymphoma
- Occurs in 1 -2 % of all lymphomas and initially found in African children and young adults (endemic). There is Burkitt-like lymphoma and they are difficult to tell apart therefore usually classified together. Endemic is rare in US
- Burkitt-like, more common in US will form a mass in the abdomen, but could start in the ovaries, testis, and other areas. It spreads to the spinal cord and the brain. 90% are males and usually around the age of 30
- Lymphoplasmacytic lympohoma
- Occurs in only about 1 - 2 percent of the population
- Small and usually found in bone marrow, lymph nodes, and spleen
- Hairy cell leukemia (HCL)
- Considered a lymphoma and rarely occurs. Approximately 700 people are diagnosed a year in the US
- Protrusions from the diseased B-cell is why its call "hairy"
- Slow growing and if treatment occurs is usually effective
- Primary central nervous system lymphoma
- Usually seen in the brain, but might be found in and around the spinal cord and can spread throughout the central nervous system
- Rare, but more common with patients that have a compromised immune system
- It has a poor prognosis
- T-cell lymphomas
- There are many subtypes and accounts for less than 15% of all lymphomas and there are many varieties. Only some of them will be mentioned
- Cutaneous T-cell lymphomas starts in the skin (example)
- Adult T-cell leukemia/lymphoma may occur when the patient is infected with a HTLV-1 virus. Less common in the US. Other subtypes include: smoldering, chronic, acute, and lymphoma
- Anaplastic large cell lymphoma (ALCL)
- This uncommon for effects children and young adults, but has been seen in people that are in the 50 - 60 year range
- Other forms of this include: skin and systemic
- FDG uptake occurs with Non-Hodgkin's lymphoma (NHL) and Hodgkin's Lymphoma (HD)
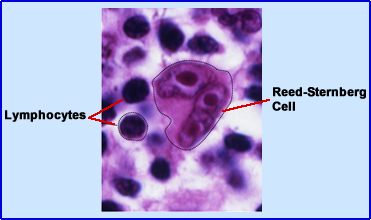
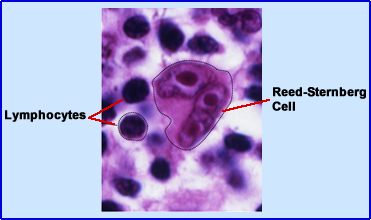
- The difference between NHL and HD is found under the microscope where Reed-Sternberg Cells diagnosis HD
- High and moderate grades of disease indicate the use of FDG in staging and evaluation of treatment outcomes
- Low grade tumors show poor uptake of FDG which may indicate the inability to stage this diesase2
- More recently Weiler-Sagie, et al stated that FDG avidity is extremely high in the following lymphomas: Hodgkin's, Burkitt, mantle, nodal marginal zone, lmyphoblastic, large B-cell, follicular, T-cell, and lymphocytic. Extranodal marginal zone lymphoma was only 55%. 21
- Staging NHL
- Biopsy has limitations in its ability to stage disease based on the difficulty of finding the involved lymph nodes. Failure to establish disease can result in the inappropriate staging and treatment
- CT has its limited abilities to determine disease based on its morphological presentation
- FDG with CT is the preferred diagnostic modality
- PET is signficantly more sensitive in finding disease when compared to CT for its based staging
- A limited amount of false-positive were found with FDG, however, a reason was not given. Can you suggest what may have caused a false positive?
- Extranodal disease
- Correlation between CT and PET showed additional disease where there are areas of FDG avidity
- Limitation with FDG is seen when evaluation bone marrow involvement, blended with PET missing low-grade and aggressive tumor infiltration
- When comparing PET with bone scintigraphy additional tumor sites were discovered with FDG
- Accuracy with PET in identifying HD and NHL shows that its utilization is cost-effective with staging, restaging, and assessing treatment outcomes
- Application of 11C methionine
- Methionine and FDG find the majority of disease, were FDG may have an advantaging in determining the difference between high and low grade tumors
- Methionine greatest advantage may be with patient that are hyperglycemic
- Subtypes of HD and the potential of staging
- Between all the detail one must conclude that PET should be routinely used for staging HD
- Limitations of PET may include
- Smaller tumors (1cm or less) generating a false negative scan
- Lymph node involvement can be assessed with PET, however, extranodal may have some limitations (size?)
- If PET shows additional lesions, biopsy should be done to those area to confirmation disease
- Low-grade HD
- There is conflicting data with FDG's ability to define low grade tumor, however, uptake of this radioisotope does occur and is used in staging
- Biopsy with PET should improve patient management with these disease sub-types
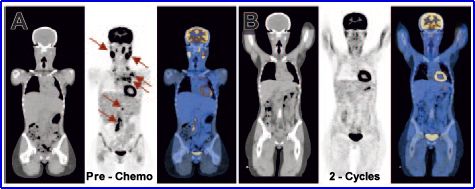
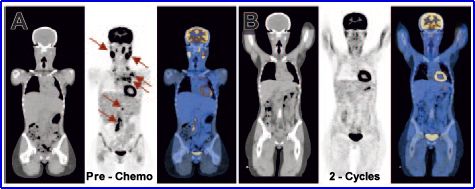
- Application of PET to evaluate the treatment of HD and NHL
 20
20
- The amount of cycles and the degree of FDG uptake does define chemotherapy's ability to treat disease. If the SUV remains the same or is higher following one or more cycles then treatment must be modified (because it's not working). The above example a patient had a baseline PET scan followed by a second after 2 cycles of chemotherapy. CT shows swelling in some of the involved nodes, however, PET showed normal uptake. After treatment, a four year follow up, the patient is still in remission
- During chemotherapy when FDG uptake (SUV) decreases, this indicates that the therapy is effective
- The lack of FDG uptake does not preclude the presence of residual disease at the micro level (occult)
- Research indicates that when PET is negative at the end of chemotherapy the probability of relapse of disease at 18 to 38 months is minimal. (e.g. - Mikhaell et al. found that 2 of 23 patients relapsed @ 38 months post therapy)
- False positives have been reported and are related to inflammatory lesions. For this reason, biopsy is recommended to confirm the presence of cancer
- Follow-up and post therapy
- Jerusalem G, et al. evaluated a group of patients that completed their chemo/radiation therapy for relapse of lymphoma. Only five patients were FDG avid after his/her therapy was completed. For a 3 year period after therapy these 36 patients were periodically exam with follow-up PET scan. Cancer returned on all 5 patient FDG avid patients
- In this same group 6 patients had false-positive scans which was thought to be inflammation, but later was discovered a hyperplastic thymus gland
- 67Ga was also mentioned as a reliable predictor to evaluate patients with HD and NHL
- Melanoma (example)
- This is the fastest gowning cancer in US and Western Europe that has a high mortality rate. Patients with regional lymph node involvement have a 20% cure rate, whereas distal mets have none
- This is a very aggressive cancer and has its best cure rate when it is found and surgically removed at the local level
- It can spread anywhere in the body via the lymphatic and/or vascular systems
- Mean survival for distal mets is 4 to 6 months
- Conventional methods to stage disease
(two methods)
- Breslow thickness defines the thickness of the cancer and determines if anything is greater than or equal to1.5 mm in thickness it usually indicates the tumor has gone beyond its primary site (This seems to be the preferred method of staging)
- Clarks methods classification (second type of staging) looks at the depth of the tumor and relates it to its involvement with dermal to subcutaneous fat
- Ultrasound, CT, and chest x-rays have high false positive/negative rates
- When compared to all other cancers FDG has its greatest SUV values with melanoma
- As a general rule, any patient that has a Breslow thickness of 1.5 mm or greater should be a candidate for FDG
-PET
- Sensitivity/specificity are around 90%/87%
- Staging by PET is cost-effective when compared to other modalities and has changed patient management
- False-positives are most often seen in inflammation or post surgical sites
- False-negatives may occur with slow growing tumors that are mostly composed of necrotic tissue
- Metastatic disease can also find it in brain and lung, with the high uptake of glucose in the brain making it difficult to see
- Bone and Soft Tissue
- There are multiple types of tumors which are derived from mesenchymal tissue (cells that come from connective tissue, blood, and bone)
- Malignant tumors include: asymptomatic cartilaginous neoplasm, chodrosarcoma, Ewing sarcoma, osteoscarcoma, with the key word being sarcoma
- Benign tumors include: enchondroma, Giant cell tumor, fibrous dysplasia, and hematogenous osteomyelitis
- Methods of staging these diseases
- CT, MRI, and sometimes ultrasound are the more common methods for evaluating disease involvement
- Where disease is found histologically workup becomes essential in determining the extent of disease
- FDG
- in bone (N18F compared to 99mTcMDP - example)
- Very useful in finding primary in all high grade malignancies (sensitivity 93%)
- Poor uptake was is seen with low-grade chondrosarcomas with a specificity of 67% (high false negatives)
- False-positives were noted in Giant cell tumor, fibrous dysplasia, and osteomyelitis
- FDG was found to be better than MDP bone imaging in the evaluation of tumor response (osteoscarcoma and Ewing sarcoma)
- FDG - soft tissue
- Gastrointestinal stroma (GIST) re best seen with CT, MRI, and PET. Ronellenfitsch, et al, identified the importance of FDG PET with deciding on whether or not to perform surgery, based primary vs. metastatic growth22
- With intrapulmonary lesions PET-FDG uptake does not occur
- PET seems to assist in the ability to grade the tumor which is based on the SUV value
- Liposarcoma was 91% sensitive and 88% specific
- Low grade sarcomas uptake with FDG is equal to muscle
- FDG's use in the evaluation of therapy
- Schirrmeister et. al found that initial staging was improved with FDG when compared to MRI and CT in evaluating multiple myeloma and solitary plasmacytoma (these are malignant plasma cell soft tissue tumor) FDG found 60.9% more lytic bone lesions when compared to x-ray
- FDG was able to show whether or not this chemotherapy agent was being effective
- PET seems to be effective in: grading, follow-up, post treatment, and detection of distal mets
- Tumors that have an unknown primary
- By definition, a tumor that has been biopsied, cell type(s) defined, and clinical workup (imaging) completed may still have a an unknown primary. This occurrence may be as high as 15% in certain patient populations
- Reasons why the primary
cannot be found
- Primary Occult tumor may be to small to identify - eg. resolution issue
- In theory, the body may have already destroyed the primary site, making it impossible to find the primary
- Where do some of the primary cancers come from?
- Axillary mets originating from the breast
- Neuroendocrine and gastrointestinal cancers spreading to the liver
- Squamous cell cancer of the tonsils are found on the neck
- Base of the tongue, pyriform sinus or nasopharynx primaries are difficult to find (size)
- Cervical metastatic disease that comes from adenocarcinoma may originate in: thorax, gastrointestinal, or urogenital
- Role of PET
- Most studies have shown that PET is not very useful in this arena, however, this may be do to the fact that PET has been the procedure of "last resort." Following this form of patient management PET has shown limited statistically impact
- However, if PET was done prior to all other clinical procedures, it might "lead" the evaluation process to determine which other types of clinical procedures
are needed to find that hidden primary
- This type of utilization may be a more cost-effective (reducing the amount of other clinical procedures)
- Specific subgroups of disease might be quickly identified, such as, metastatic disease in the neck defined as adenocarcinoma
- Factors to consider are: the type cell type found on biopsy and the location(s) of the metastatic disease
- This method is used at MCV
- Elboga et al evaluated 112 patients, of which FDG PET was able to identify primary tumor, find new metastatic sites, and change the clinical treatment of 1/3 of the patients in this study23
- Brain cancers will be covered under the Brain lecture
- Concluding comments based on an article that was published in 2008, "Recommendation on the Use of 18FDG PET in Oncology" by Flecher JW, et al. (a must read article)
- PET should be used along with other imaging systems (MRI and CT)
- Positive finds leads to
- Changes in the clinical management of patients
- Histologically correlation should be done, due to false-positive results that may occur with FDG
- Use FDG-PET to initially diagnosis: head and neck, lung, pancreatic cancers, and unknown primary tumors
- In the area of staging PET should be used in: breast, colon, esophageal, head and neck, lung, lymphoma, and melanoma
- Finally, PET-FDG should used when recurrence is suspected in the following cancers: breast, colorectal, head and neck, thyroid, and lymphoma
- Mixed cell cancers tend to have poorer FDG uptake
- Throughout the literature I have seen comments stating "there is limited data" on this topic. I found this particular true when it came to radiopharmaceuticals that have short half-lives. If you think about it its the T1/2 issue that makes some of these PET agents difficult to work with and therefore difficult to accumulate enough data to make appropriate conclusions
Return to the Beginning of the Document
Return to the Table of Content
1 - The expanding role of PET technology in the management of patients with colorectal cancer by Herbertson, et. al.
2. The impact of fluorodeoxyglucose-positron emission tomography in primary staging and patient management in lymphoma patients by Allen AuebackM, et al.
3 - The predictive value of positron emission tomography
scanning performed after two courses of standard
therapy on treatment outcome in advanced stage
Hodgkin's disease by Gallamini A, et al.
4 - 18F-FDG Positron Emission Tomography CT (FDG PET-CT)
in the Management of Pancreatic Cancer: Initial Experience
in 12 Patients by Saif MW, et al
5 - C-11 choline PET/CT imaging for differentiating malignant from benign prostate lesions by Li X, et al
6 - Positron emission tomographic imaging of acoustic neuromas. Sakamoto H, et al, (2000) Acta Otolaryngol Suppl[TA]
7 - 18F-FDG PET/CT in primary central nervous system lymphoma in HIV-negative patients. Karantanis D, et al. (2007) Nucl Med Commun
8 - [18]FDG-PET in patients with in situ breast carcinomas. A cause of false negative results]. Ruibal A, et al., Med Clin 2008 (Brac)
9 - High-resolution fluorodeoxyglucose positron emission tomography with compression ("positron emission mammography") is highly accurate in depicting primary breast cancer. Berg
WA et al.
(2006) Breast J
10 - Preoperative assessment of hilar cholangiocarcinoma by dual-modality PET/CT Jun Li, et al. (2008) Wiley Interscience
11 - Clinical Applications of PET in Brain Tumors. Chen, W (2007) JNM
12 - Prognostic Value of 18FET and MRI in Small Nonspecific Incidental Brain Lesions, Floeth, FW, et. al., (2008) JNM
13 - Is 18F-FDG PET/CT useful for distinguishing between primary thyroid lymphoma and chronic thyroiditis? Nakadte M, et. al Clin Nucl Med 2013
14 - Unfolding the role of PET FDG scan in the management of thyroid incidentaloma in cancer patients, Gavriel H, et al. Springer 2014
15 - Appropriate use of positron emission tomography with [18F]fluorodeoxyglucose for staging of oncology patients, Tagilabue L, et al Internal Medicine 2013
16 - PET/CT in the Management of Thyroid Cancers, Marcus C, et al NM and Mol Imaging
16. - PET scan for a hepatic Mass, Blechacz et al. Hepatology (2010)
17 - Utility of PET/CT in diagnosis, staging, assessment of resectability and metabolic response of pancreatic cancer, Wang et. al. (2014)
18. - 18F-FDG PET for the identification of adrenocortical carcinomas among indeterminate adrenal tumors at computed tomography scanning, Nunes, et al. 2010
19 - The role of PET/CT in cervical cancer by Fernanda, et al (2013)
20 - FDG-PET after two cycles of chemotherapy predicts treatment failure
and progression-free survival in Hodgkin lymphoma by Htuchings, et. al (2006) ASH
21 - 18F-FDG Avidity in Lymphoma Readdressed: A Study of 766 Patients by Weiler-Sagie, et al. JNM (2010)
22 - [Importance of PET for surgery of gastrointestinal stromal tumors], Ronellenfitch Chirurg (2014)
23 - Utility of F-18 fluorodeoxyglucose positron emission tomography/computed ın carcınoma of unknown primary, PMC (2014)
The majority of this lecture references are from: von Schulthess G K (2003) Clinical Molecular Anatomic Imaging. Lippincott Williams & Wilkins, pp. 150-174 and 251 - 398
 16
16
 20
20
