- Anatomy and physiology of the kidney
- Pre-renal
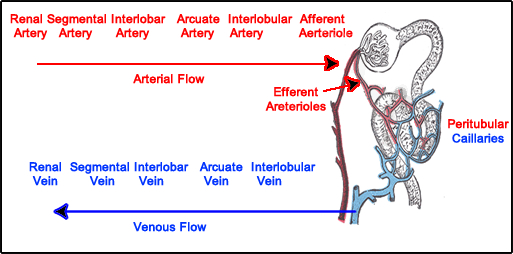
- Blood flows down the descending aorta to the abdominal aorta
- Branches at the renal arteries
- Supplies blood to the left and right kidneys
- Blood arrives at the kidneys and receives approximately 20 - 25 % of the cardiac output
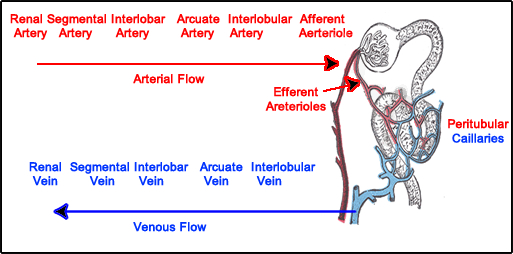
- Renal artery enters the kidney and subdivides into the segmental artery, which goes to the 8 different Calyxes
- In each renal calyx arterial blood flow branches as follows: interlobar arteries, arcuate arteries, interlobular arteries, to the afferent arterioles
- Nice diagram of renal arterial blood flow (click it)

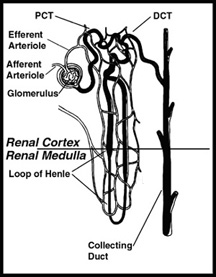
- Afferent arterioles supplies the glomerulus (bowman's capsule)
- Leaving the glomerulus the blood travels through the efferent arteriole with a network of peritubular capillaries that surround the convoluted tubules and loop of Henle
- Capillaries converge into interlobular vein, arcuate vein, interlobular vein, that feeds into the renal vein
- Nephron physiology (Intra-Renal)
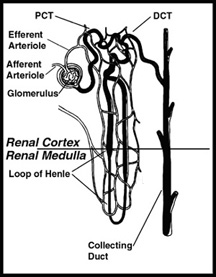
- The entire structure can be seen in the diagram below
- Blood enters the nephron from the afferent arteriole at the Glomerulus/Bowman's capsule
- Where 20% of the cardiac output arrives at approximately 1.2 L/min
- One can make an assumption that 50% of whole blood is plasma, hence the Effective Renal Plasma Flow (ERPF) value would be 600 mL/min
- About 20% of this plasma is filtered by the glomeruli resulting in a glomerular filtration rate (GFR) of 120 mL/min
- This 20% is also know as the filtration fraction which is derived GFR/ERPF
- 120/600 = 0.2 or 20%
- Most of the filtered plasma is reabsorbed
- Glomerulus is the first step in urine formation
- Waste products, electrolytes, and water are filtered out by the proximal convoluted tubule
- These by-products are then sent down the Loop of Henle and exit out the distal convoluted tubule
- Certain by-products may re-enter or be reabsorbed along this tubule via the peritubular capillaries
- The excreted by-products or urine that remain in the tubules continues out the collecting ducts and then enter the ureter
- Between the afferent and efferent arterioles is the juxtaglomerular apparatus
- This structure response to renal artery stenosis (RAS) and low sodium concentrations
- It secrets rennin that starts the process of producing angiotensin, which when applied vasoconstricts the efferent arteriole
- This process will occur with a patient that has renal artery stenosis. The body attempts to equalize the pressure by constricting the efferent arteriole (the process will discussed further under captopril renogram)
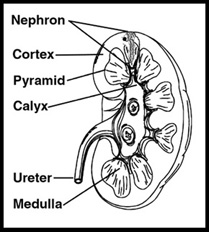
- Kidney
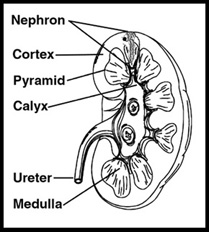
- Identify the location of the nephron within the kidney
- Note the other sections of the kidney: Cortex, pyramid, medulla, calyx, and ureter
- It is important to understand these structures when drawing the appropriate ROIs in a renogram
- Lasix renogram includes the entire renal pelvis
- Captopril (ACE inhibitor) renogram requires the ROI to only be drawn around the renal cortex
- Lasix and Captopril will be discussed in the future
- Radiopharmaceuticals used to image the kidney
- Glomerular Filtration Rate (GFR)
- As blood and plasma pass through the glomerulus, approximately 20% of the plasma is filtered out at 120ml/minute (as noted above)
- Best agent to quantify GRF is 99mTcDTPA
- Only 3 to 5 % of this agent is protein bound, which results in a small error in the GRF value (if the error is known then this can be added to the calculation)
- Increased rennin flow increases protein binding which falsely lowers the GFR
- T1/2 for DTPA are: 10, 90, and 600 minutes. In further assessment Sodee1 states that less than 10% remains in the blood at 2 - 3 hours
- Reducing agent in the DTPA kit is ascorbate which increases cortical binding of the agent (what happens to the GFR calculation if there is too much cortical binding?)
- A dynamic imaging procedure is used to identify the passage of the radiopharmaceutical through the kidneys
- Quantitatively, ROIs are drawn around the kidneys and time/activity curves is generated, which define renal function of the radiotracer passing through the kidneys
- Effective Renal Plasma Flow (ERPF)
- Identifies the amount of plasma that is filtered by the kidneys = 600 mL/minute
- Agents used to quantify ERPF are 131 HIPP and 99mTcMAG3
- MAG-3 is the agent of choice
- Tubular agents (radiopharmaceuticals) are used to determine ERPF
- OIH is similar to paraaminonohippuric acid (PAH) which is the gold standard to determine ERPF (PAH is not an NMT procedure)
- OIH - 80% is filtered by the tubules and 20% is filtered by the glomeruli
- Jolles states that MAG3 filters 10% GFR and 90% EFPF
- Clearance depends on the extraction efficiency and the blood flow to the kidneys
- OIH - 96% is extracted from the arterial blood
- OIH - Extraction fraction is approximately 65% at first pass with 70% cleared from the vascular pool in 30 minutes
- In normal renal excretion maximum concentration occurs in the kidney at 3 - 5 minutes with 50% remaining at 7 - 10 minutes
- Most of MAG-3 is excreted through the proximal convoluted tubule
- MAG3 is not extracted by the kidneys as efficiency as OIH
- In comparison of I131-OIH to MAG3
- Rate of clearance 1.301/minute (MAG3) and 0.881/minute (OIH) - normal volunteers (NV)
- Research has shown that renogram curves and 30 minute excretion rates were similar in NV
- Image quality for MAG3 was significantly better than OIH (why?) - NV
- Note I131-OIH dose is ~ 300 μCi and Tc99m-MAG-3 is ~ 10 mCi
- MAG-3 is the superior agent in patients with renal impairment (RI)
- 30-minute excretion was about the same for both (RI)
- Time to peak was more rapid with MAG3 (RI)
- MAG3 is 90% protein bound
- MAG3 is 5.1% bound to RBC, while OIH was 15.3%
- MAG3 may show hepatobiliary uptake (and GB)
- Does hepatic uptake effect quantification?
- Peak for both is between 2.5 to 3.4 minutes
- Quantitatively, ROIs are drawn around the kidneys, and a time/activity curves is generated which displays renal function of the radiotracer passing through the kidneys
- Perfusion image for static analysis
- Identify space-occupying lesions
- Agent of choice is 99mTcDMSA
- Considered a parenchymal imaging agent
- 90% is bound to serum protein
- Extraction fraction in to tubules is around 4 - 5%
- 50% adheres to the tubules at 1 hour post dose
- DMSA molecule splits when it reaches the kidney, in which part of it is secreted and part it binds to the tubules
- DMSA expires 4 hours minutes after its reconstituted
- Radiotracer perfuses into the kidneys and is retained by the renal cortex which allows for examination of renal anatomy
- Perfusion and quantification
- 99mTc-glucoheptonate (GH) can be used for either cortical imaging and renal function
- 50% is bound to the plasma protein
- Tubules to glomeruli extraction is about 50/50
- 10% binds to the renal cortex in 1 - 2 hours
- Early analysis of the renal procedure yields function, however, delayed images better defines renal anatomy
- Considering the above outline, how would you use these radiotracers to & image the kidneys?
Return to the beginning of the page
Return to the Table of Contents
6/15
Principles and Practice of Nuclear Medicine by PJ Early and DB Sodee, 2nd edition