- Trauma (fx)
- A patient that is < 65 years old, an has no osteoporosis, will have a positive bone scan 95% of the time in 24 hours and nearly 100% in 72 hours.
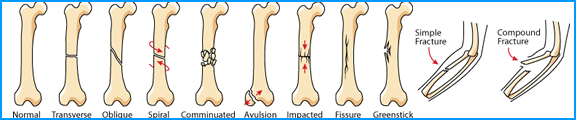 Types of Bone fractures - http://askabiologist.asu.edu/how-bone-breaks
Types of Bone fractures - http://askabiologist.asu.edu/how-bone-breaks
- The older the patient, the longer it takes for the scan to be positive when an fx occurs.
- Imaging fx and the stages of recovery:
- The first stage has fairly diffuse increased activity about the site that lasts 2 to 4 weeks
- The second stage has a well demarcated linear zone of increased activity at the site and last 8 - 12 weeks post onset
- The third stage bone eventually turns to normal (90% in 2 years and 95% in 3 years).
- It may also be impossible to distinguish pathological fx from simple traumatic collapse (ex. collapsed vertebrae)
- A patient that is < 65 years old, an has no osteoporosis, will have a positive bone scan 95% of the time in 24 hours and nearly 100% in 72 hours.
- Stress fx
- It has been generally believed that stress fx is more painful than most other types of fx. However, Groshar's study showed that 25% of his patients that had stress fx had no associated pain
- Stress fx may be multiple in nature and may occur in tib/fib as well as other areas of the body. Other bones would include hands, feet and long bones of the arms and legs
- The Periosteal stress reaction is the formation of new bone that respond to injury. Periosteal stress reaction never becomes abnormal on x-ray, heals more quickly than an fx, and returns to a normal bone scan at a faster rate
- Clinically, the best time to take an image is 2 weeks post onset of pain. The regions that extend 50% or more into the cortex are called stress fx (or significant extension into the cortical bone). Less than 50% is called primary peripheral lesion (periosteal stress reaction)
- Continued stress on the bone (ex. running) may result in aseptic necrosis
- An example of a pre-stress fracture is a result of excessive exercise. Continued abuse may lead to a stress fracture
- Viability of bone following trauma
- Avascular necrosis (AN) is a common complication of the femur, carpal or navicular bone(s)
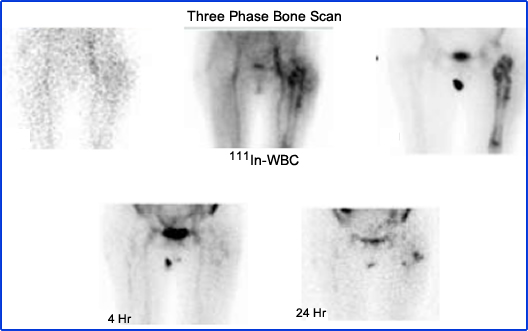
- Viability of the femoral head following fx in or above the neck of the femur is of great concern. In a three phase bone scan, loss of activity seen in the first part with a photopenic area on the delays is a strong indication of AN
- How would we image this type of patient? Think pinhole or SPECT
- Non-union of fractures
- Bone imaging is preferred over radiographs in the detection of non-union fx. However, neither x-ray or nuke can distinguish between delayed healing and non-union. This occurs about 5 % of the time with patients that have compound or communicating fx. (see types of fractures)
- Other factors that may cause non-union are: inadequate blood supply, osteoporosis, infection; Hyperparathyroidism, and poor nutrition
- Atrophic non-union causes a reduction in tracer activity at the affected site. Pinhole imaging may identify the lack of activity at both edges of the bone where the fx has occurred
- Reactive non-union shows increased activity at the area of interest, which indicates possible callous formation. However, the bone does not knit. This may be due to an infection, or it may just be delayed nonunion. In this case, there would be a lack of activity
- Ga67 or labeled WBCs may be used to analyze reasons for delayed or lack of healing
- Grafts
- Bone imaging is extremely sensitive in evaluating new bone growth. Viable grafts show increased activity in every stage, whereas nonviable will have reduced flow and decreased activity on delays. In dogs, a nonviable graft would take an additional 3 - 6 wks before radiographs become positive.
- Prostheses
- Postoperative evaluation of prosthetic devices and the use of bone imaging are controversial. It is difficult to differentiate between heterotropic bone formation, prosthetic loosening, and infection (they all look hot).
- Gallium or Indium may further assist in evaluating "loosening with" vs. "loosening without" infection.
- When loosening alone is present, activity is seen in the area surrounding the prostheses. If Gallium- or Indium-labeled white cells are injected, an infection will pick up the radiotracer
- Radiographic studies sometimes identify loosening however, a normal or equivocal x-ray would require additional investigation

- Child abuse
- Traumatic disruption of the periosteum is more common in children than in adults.
- The problem is the extensive amount of bone growth in an infant and the acute trauma within the same area
- Common traumatic injuries include: epiphyseal fx, epiphysitis (especially the elbow), apophysitis (especially the insertion of the Achilles tendon), trauma around the pelvis and spine
- Bone imaging in nuclear medicine will give significantly less radiation exposure when compared with a skeletal survey
- Package insert MDP

- Avascular Necrosis (AVN) [this is something I've never seen done - but recommended in the literature]
- Is this caused by a loss of blood supply to the femoral head. Some conditions that cause this are: leukemia, septic joint condition, hemorrhaging
- The key to identifying AVN is to do a bone scan when there is a sudden onset of pain in the affected area. If done later, it may be difficult to identify AVN from bone formation and re-vascularization
- Four stages/patterns in the healing of avascular necrosis
- Early stage demonstrates absent activity in the affected area. X-ray looks normal. This condition is noticed within 5 weeks of onset
- Stage II has early re-vascularization, and this usually takes about four months
- Stage III, or "base filling," occurs around 10 months with a diffused zone of increased activity
- Stage IV occurs when the bone returns to normal with a timeframe of 18 - 24 months
- SPECT and MRI are also suggested
- Complete healing cannot be noticed if the patient has an aseptic femoral head
- Photo-deficient areas may also be due to: vasculitis, infarction (sickle cell), neoplasm, alcoholism, lupus, steroid therapy, and impaired circulation (diabetics and frostbite)
- The Wrist, ankle, feet, knees, and humeral head may also have AVN

- Arthritides/Arthritis
- A whole body bone scan is the method of analyzing all articulating processes and may show arthritis before radiographic images
- While MDP is usually administered to the patient, 99mTc04- or 99m TcHSA (no longer available in US), may be considered to differentiate between rheumatoid arthritis (synovial inflammation) and degenerative osteoarthritis. Shortly following IV administration of either of these radiotracers, synovial inflammation (soft tissue) will show increased activity; however, degenerative osteoarthritis will show normal distribution (this would be in a dynamic or pooling phase)
- A three-phase bone scan will show arthritic condition, and synovial involvement shows increased uptake in the joint at all three phases
- Cellulitis that has no osteomyelitis involvement will only have uptake in the first two phases of a three phase bone scan
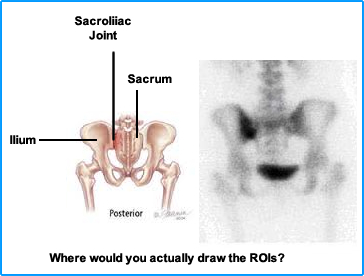
- Quantification of the sacroiliac (SI) joint to identify inflammatory sacroiliitis:
- Acquire a posterior pelvis image and draw regions of interest around the hottest area of the L or R SI and around the mid-portion of the sacrum.
- Abnormal region counts are then divided by Normal region counts = Bone concentration ratio
- 1.1 to 1.55 = Normal
- 1.55 to 1.75 = equivocal
- Greater than 1.75 = inflammatory sacroiliitis
- Profile slices have also been done, but the above is the recommended procedure
- Ankylosing spondylitis (AS) is a chronic soft tissue inflammation process involving the sacroiliac and vertebral joints but may include the peripheral joints, sternum, and costochondral junctions. A pattern of focally increased activity in the vertebral body indicates fx where decreased uptake in the areas is AS
- 67Ga may be used to determine septic arthritis. However, it is hard to differentiate between both because of the superimposition of arthritis and synovitis
- Joint replacement in the knees vs. arthritis is 96% sensitive
- Types of arthritis include ankylosing spondylitis, gonococcal arthritis, gout, psoriatic arthritis, rheumatoid arthritis, scleroderma, and systemic lupus erythematosus. The five most common forms of arthritis.
- Homework - Calculate the ratio for inflammatory sacroiliitis
- Metabolic Disease
- The exact role is not always unclear. Usually there is increased bone uptake in the area that has the involved disease
- Hyperparathyroidism shows increased bone involvement everywhere, which even includes the phalanges to tarsals. This is due to the secretion of PHA, which causes high bone turnover
- Paget's will show increased involvement in the pelvis, extending down the long bone or skull
- Decreased radiotracer uptake can also be seen in osteoporosis and osteopenia, and osteitis fibrosa cystica
- An unusual case where there is a combination of hyperparathyroidism and osteitis fibrosa cystica
- The exact role is not always unclear. Usually there is increased bone uptake in the area that has the involved disease
- Irradiated Bone
- Irradiation of bone will initially show increased tracer uptake until it reaches a threshold level, at which point the area will become photopenic
- In one study 4 - 6 months post-dose, 60% had photopenic patterns had a mean of 3750 rad delivered. No changes occurred when the dose was less than 2000 rad.
- Bone activity usually returns in 12 months but may take up to 2 years
- Infection
- In acute osteomyelitis, a three phase bone scan is recommended. It is also much more sensitive than radiographic techniques
- Increased soft tissue uptake and slightly increased or normal activity in the delays indicates cellulitis
- Fungus will show increased uptake for the first two phases, but not the third of a three phase bone scan
- Cellulitis is another diagnosis that will only show increased uptake in the first two phases
- Focal abnormally in all three phases is indicative of osteomyelitis
- Note the reason to do a fourth phase, as we've already discussed
- Radiography is 78% accurate, while the three-phase is 94%
- Neonates and elderly with poor peripheral vascularity are also poor three-phase candidates
- Chronic osteo may be difficult to image, and 67Ga should improve our diagnostic ability
- A slight increase or normal three-phase and increased Ga67 is considered a positive study
- In chronic osteo, 111InWBC is not recommended
- 67Ga or 111In increases sensitivity and specificity in the detection infection
- The Sensitivity of 111InWBC may be reduced if antibiotics were administered
- Early osteo has seen cold spots in the affected area, which may be due to an interruption of blood supply. Infarction (sickle cell disease) may also be photopenic
- Following Ab therapy, if the bone agent is decreasing in serial imaging, then the thx is effective. 67Ga may stay hot longer than 111In-WBC, in analyzing the therapeutic response
- If you want to know more about 67Ga or 111InWBC click this link. We will discuss these tracers in detail during your senior year
- Soft tissue accumulation
- Soft tissue background increases with age
- Diffused increased activity and/or ureter uptake indicates possible renal obstruction. Remember, with bone imaging and renal uptake there may be serendiitous findings such as space occupying-lesion, lack of renal uptake, or ureter blockage
- Infarcts in the heart, brain, gut, or muscle may show increased uptake
- Electrical burn
Return to the beginning of the document
Return to the Table of Content
Continue to the Next Lecture