- Nuclear medicine has three methods of examining the thyroid
- Iodine uptake
- Thyroid Imaging
- Pharmacological stimulation
- There are three types of radiopharmaceuticals used to determine the uptake and/or imaging of the thyroid gland
- 123I
- 131I
- 99mTcO4-
- When administering the specific radiopharmaceutical radiation dosimetry must be considered
- A 200 μCi dose of 123I will deliver 2.6 rads to the thyroid and 6 mrads whole-body
- A 50 μCi of 131I will deliver 65 rads to the thyroid and 23 mrad whole-body
- Why is the 123I dose so much greater than the 131I dose?
- If a 200 μCi was a administered to the patient how much radiation would the thyroid get?
- A 10 mCi dose of 99mTcO4-will deliver 0.6 rad to the thyroid and 70 mrad whole-body
- Quick review of the uptake procedure
Radiopharmaceutical used for thyroid uptake and/or scan
Radiopharmaceutical |
123I |
131I |
99mTcO4- |
Physiology |
Trapped/organified |
Trapped/organified |
Trapped |
Gamma/beta |
Gamma |
Gamma/beta |
Gamma |
Dosimetry |
Low |
High |
Low |
T1/2 |
13 hours |
8 days |
6.02 hours |
KeV |
159 |
364 |
140 |
Uptake/image |
Both |
Both |
Image only |
Therapy |
No |
Yes |
No |
- Thyroid uptake
- There are two basic formulas/procedures to consider when determining thyroid uptake
- The formula/procedure you learned last semester is as follows
- Count thyroid pill in thyroid phantom using uptake probe (distance 20 cm) = Pill count at 0 hr (phantom simulates neck attenuation)
- Count Room at 0 hour = Bkg1
- Dose patient
- At twenty-four hours post dose, take patient bkg by counting the thigh = Bkg2
- Count the patient thyroid at 20 cm at twenty-four hours = Patient thyroid at 24 hrs
- Apply formula (see below)

- Example of 123I thyroid uptake calculation:
- Pill count at 0 hr = 1,545,667 cpm
- Bkg1 = 132 cpm
- Patient's thyroid count at twenty-four hours = 215,558 cpm
- Bkg2 = 2,154 cpm
- Answer = 49.6% or 50%
- Decay factor = 0.278
- 1,545,667 - 132 = 1,545535 (net counts a 0hr)
- 215,558 - 2154 = 213,404 (net thyroid counts at 24 hr)
- 1,545,535 x 0.278 = 429,864 (pill count adjusted for 24 hr decay)
- (213,404/429,864) x 100 = 49.6 % uptake
- A different formula maybe considered (see formula below)

- This formula considered the use of a standard pill (S1) and a patient pill (P1) where both pills are counted in the thyroid phantom, however, P1 is administered to the patient while S 1 is stored for counting at 24 hours
- Room background is counted and subtracted into S1 and P1 in order to obtain net counts of both S1 and P1
- At 24 hours the standard is counted within the thyroid phantom (S2) in order to determine the decayed pill count
- Patient's thyroid is counted at 24 hours and this becomes (P2)
- Patient's thigh is counted and this becomes the patient?s background
- P2 - pt Bkg = net thyroid counts
- Room background is count at 24 hours
- S2 - Rm Bkg at 24 hours = net pill count at 24 hours
- Example of 123I thyroid uptake using a standard pill
- S1 = 1,545,667 cpm
- P1 = 1,511,144 cpm
- Room background at 0 hours = 132 cpm
- Net S1 = 1,545,535 cpm
- Net P1 = 1,511,012 cpm
- Patient thigh counts at 24 hours is 2154 cpm
- Room count at 24 hours is 159 cpm
- P2 (net) = 210,633 - 2154 = 208,479 cpm
- S2 (net) = 419,547 - 159 = 419388 cpm
- Thyroid uptake is then 51%
- General comments regarding the application of the two thyroid uptake formulas
- Keep distance constant for all counts: from the phantom, thigh, and thyroid. A distance bar attached to the uptake probe should be used to assure a constant distance
- Time for each count may range between 1 to 3 minutes (keep constant). However, when using 131I a 3 minute count is suggested in order to maintain appropriate counting statistics
- Use the decay formula with the appropriate iodine
- Decay formula is not required if a standard pill is being used
- If the time varies greater than +/- 15 minutes from the 24 hour count, then adjust the decay formula when using 123I.
- Why is the above statement not as important when using 131I?
- Comments regarding the use of a standard pill
- Decay formula does not have to be used. Why?
- If there is a slight change in the counting equipment's high voltage from one day to the next, this formula would maintain counting accuracy
- If your counting equipment fails at the time the 24 hour count then a substitute counting system maybe used and thyroid uptake can still be determined
- Don't make this mistake - I have seen a department only count the count P1 believing that the activity in S1is the same (it is not!). Therefore, the cpm values of both S1 and P1 should be similar. While all thyroid pills are calibrated for 12N there will still be a slight μCi variation from each pill. What is the dpm of 1 μCi? Assume a 30% counting efficiency. If there is a 1 μCi difference then this will falsely effect your % uptake results?
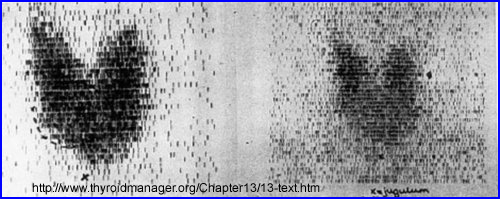
- Thyroid Scan (for more detail see Thyroid Procedure):
- Matrix size for 123I or 131I = 128 by 128 )
- Matrix size for 99mTcO4- = up to 256 by 256
- Pinhole collimator
- Views: ANT; ANT with marker; RAO; and LAO
- 25 to 50k counts with iodine
- 100 to 200k counts with 99mTcO4-
- ANT marker view - mark the sternal notch and all nodules
- The physician should palpate the thyroid and mark each nodules with a black marker so that the technologist can label it with a radioactive source
- Marking the nodule - Two methods
- Take the 57Co flexible ruler and circle all the palpable/marked nodules and acquire the ANT marker image. This will assist in determining whether the nodule is extrinsic or intrinsic to the thyroid
- Another method for marking nodules is to take a small amount of technetium activity and place it at the end of a 1 cc syringe (located in the hub of the syringe). Remove the needle and replace it with syringe cap to prevents contamination. With the radioactive "wand" highlight each nodule that was identified by the physician by placing the tip of the wand over the each nodule for about 3-5 seconds and acquire the data


- Other Thyroid imaging procedures
- TSH suppression test
- In the presence of an autonomous nodule (Plummer's disease) the physiological response by the body is to drastically reduces TSH secretion, which should in turn shut down the thyroid gland. Normal functioning tissue does respond to reduced TSH levels, however, an autonomous nodule continues to trap iodine and procedure T3/T4 at a hyper-active rate. Therefore, in order to determine if the suppressed thyroid tissue (around the nodule) is till functioning excess levels of TSH is administered to the patient along with radioiodine. If normal tissue is visualized, then the nodule can be surgically removed with the hope that the remaining tissue will take over in a euthyroid state.
- Procedure
- Day one: Give pt 10 units TSH IM
- Day two: take bkg of thyroid (if necessary) and give 10 units of TSH
- Day two: Give 100 - 300 μCi of 123I
- Day three: Complete an uptake and scan
- Cytomel suppression study
- Used to differentiate between autonomous and non-autonomous nodules. After administering Cytomel (liothryonine) for several days, if the nodule stays hot it is considered autonomous in nature. However, following suppression, if the nodule reduces in activity then the nodule is not considered autonomous
- Procedure
- Complete a routine thyroid uptake prior to this procedure
- Give the pt 25 μg of Cytomel (liothyronine) TID for five days
- Administer 200 μCi of I123
- Complete a 24 hour uptake and scan
- Perchlorate discharge test
- Hashimoto's disease and congenital enzyme deficiencies cause organification defects. With the administration of ClO4-, it is trapped by the thyroid and displaces iodine that has not been organified. If a deficiency exits iodine that has been trapped is released in the presence of ClO4-
- Administer 20 μCi of 131I or 100 μCi of 123I
- Measure the uptake at 2 hours post administration
- Administer 1 gm of potassium perchlorate
- Take a thyroid measurement every 15 minutes for up to 90 minutes
- Normally there should be no change in the uptake, however, if a 10 to 15% or greater decrease is noted, then the test is considered positive
- Hashimoto's disease has and inhibitory effect with iodine
- Prior to WB iodine survey rhTSH should be administered. Why?
- Prior to WB survey the patient should be off thyroid supplements for 4 to 6 weeks. How do you think this makes the patient feel?
- Administering rhTSH eliminates the need to have stop thyroid supplement
- Stimulates T3/4 production and iodine uptake of residue thyroid cancer
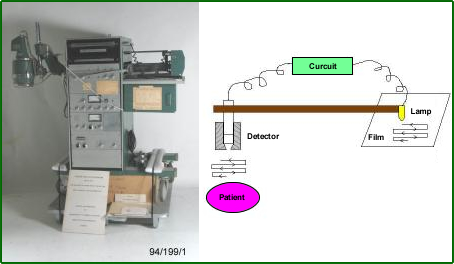
- Single probe with movable arm had the following settings
- Scan speed
- Window
- Distance between rows
- Set the count rate to the highest spot which then adjusted the gray scan
- Another look at the setup: http://en.wikipedia.org/wiki/Rectilinear_scanner
- Image
- As the probe moves back and for it sets the darkness on the film/paper based on the amount of activity in the area
- As time progresses the arm of the camera moves the detector back and forth and pending the amount of activity detected the individual dots are created, row by row, until the entire organ is imaged
- Crystal thickness varied pending the type of radionuclide used. Typically 131I was 3 inches thick and F18 would measure 5 inches
- Time for acquisition - In the worst case scenario a whole body bone scan take as much as two days to image
Drugs that effect thyroid uptake and synthesis
- Thiocyanate effects iodine trapping
- Perchlorate is similar in iodine with regards to its molecular weight and ionic charge
- Nitroprusside given to hypertensive patients and effect the trapping of iodine
- Propylthiouracil is an anti-thyroid drug specifically given to patients with hyperthyroidism.
- Tapazole is used to treat hyperthyroidism.
- Sulfonylureas - effects organification
- Sulfonamides - effects organification
- p-Aminosalicylic acid - effects organification
- Phenylbutazone - effects organification
- Aminoglutethimide used to treat adrenal cortex carcinoma Cushing's Syndrome and effects the organification process
- Iodine is also found in contrast agents used in radiology which would cause temporary saturation to the thyroid gland. It should be noted that different forms/administration of a contrast agent effect thyroid uptake for as little as several weeks (IVP) to as much or more than a year (myelogram)
- Lithium has been known to cause hypothyroidism if given over long periods of time
- Propylthiouracil - effects conversion of T4 to T3
- Glucocorticoids (steroids) decrease T4 to T3 conversion and may lead to reduced TSH production,
- Propranolol is a beta-blocker which inhibits conversion of T4 to T3. Its clinical impact is uncertain. Newer beta-blockers such as atenolol and metoprolol are cardiac specific
- Iopanoic acid (Telepaque) - See iodine
- Amiodarone is a cardiac antiarrhythmia agent which is usually given to patients with thyroid dysfunction. There is a significant amount of iodine found in this drug which effects iodine uptake in the thyroid.
How long do the following drugs effect thyroid uptake?
One week
Triiodothyronine
Thiouracils
Sulfonamides
Cobaltous ion
Thiocyanate
Perchlorate
Nitrates
Bromides
Steroids
ACTH
Isoniazid
Phenylbutazone
Thiopental (Pentothal)
Penicillin
2 - 3 weeks
Dinitrophenol Dinitrocresol Iodides
Vitamin mixtures
Some cough medications
Seaweed
Approximately 2 months
Thyroid extract Thyroxine
IV contrast media
For a year or longer
Oral contrast media
Oil-contrast media
Return to the Top of the Document
Return to the Table of Contents
Continue on with the next Lecture - Ideal Thyroid Agent
5/23