- *Know the details on how to complete a PET brain procedure
- *What concerns are there when imaging the brain with FDG - brain uptake vs. disease vs. white and gray matter
- *Up/down regulation
- Diseases:
- Application in Epilepsy
- Picks and AD
- Assessment with trauma
- Low vs high metabolic glioblastoma
- You should also note that there are numerous other radiopharmaceuticals used to image different brain diseases. For now you will only be responsible for FDG and those used to image AD
- *Metabolism
- The use of FDG in the brain can be classified as the assessment of regional metabolic utilization of glucose consumption (rCMR-glu) in brain tissue (1)
- Approximately 25% of the total energy required by the body, occurs in the brain
- Reasons for this highly metabolic rate are:
- Need to maintain ionic exchange with the sodium/potassium pump, which occurs with intra/extra cellular components of the brain
- Glucose utilization localizes around the synaptic zones
- When FDG is incorporated into the cell the above glycolysis occurs. Glucose is also included for comparison. As noted 18F is replaces an OH that presents the second phase of glycolysis to occur. Hence FDG gets trapped into the cell.
- Uptake for FDG is greater in the gray vs. white matter, however, uptake in white matter increases if there is a demand to do so

- What is the difference between white and gray matter?
- Grey matter contains your brain function, sometimes referred to as the "living brain." It contains dendrites and axon terminals of the neurons and is the location of the synapses
- White matter is made up of axons that connect the different parts of gray matter
- From a diagnostic point some brain tumors are difficult to see when using FDG. Reasons?
- FDG uptake may be greater in normal brain tissue when compared to tumor. The "background" hides the diseased tissue
- Smaller lesion with FDG uptake can be missed (based on resolution)
- The greater the metabolic activity of tumor, usually the more aggressive which also means greater uptake of FDG
- Other aspects to consider when imaging the brain with FDG
- Excessive eye movement may cause increased uptake
- Any type of outside stimuli may cause "abnormal" uptake
- Muscle and lymphatic uptake
- Resolution is PET is approximately 6 mm
- Imaging Protocol
- Place the patient in a dark quite room
- Establish an IV site at least 15 - 30 minutes prior to the FDG injection
- Inject the FDG without disturbing the patient
- Uptake phase should last 45 - 60 minutes
- The brain should be imaged in only 1 bed position
- The edges of the FOV can slightly distort an image, for this reason 2 beds is not acceptable
- Setup acquisition for 3D mode and double the acquisition time (MCV protocol) on a single bed
- When placing the head into the scanning position consider the following positioning
- Use a head holder to restrict movement may be required
- When looking at how the brain/head is position consider the above images
- From the anterior view no rotation or tilt should be seen. You should be able to draw two straight lines that are perpendicular to each other. One line through the nasopharyngeal area and the other through the orbital socket
- Lateral angle, prop up the head up several inches off the table by placing a rolled up cloth underneath the back of the skull. The slight angle improves the area to be scanned. Compare the two lateral images being displayed. The tilted brain scan takes up less space. Why might this be important?
- Sometimes, when you scan an "non-angled" image the volume of the brain will require more than 1 bed position
- If you are imaging the patient because he/she has seizures consider
- Tell the patient not to fall asleep during the uptake phase
- Connect an EEG to the patient to monitor any seizure events that might occur when he/she is being imaged

- Infections
- General (FDG)

http://jnm.snmjournals.org/content/52/6/865/F3.expansion.html- The ability to tell the difference between a high grade tumor and infection/abscess is (usually) not a problem, because tumor uptake tends to be more intense. Taking a delayed image may help
- However, a problem may occur with some infections and low grade tumors. This relates to the amount of uptake between a low grade tumors and an infectious process, where they may be similar. Furthermore, sometimes the low grade tumor and/or infection, might be masked by the normal high level of FDG uptake in normal brain tissue
- Here is an example of a brain a questionable tumor (above). Delayed imaging shows increased uptake in the area of interest define it as a tumor
- Reduced activity on delayed imaging would identify infection
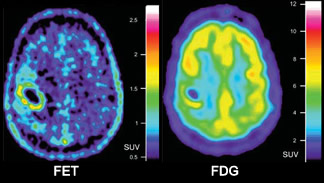
- *Here is an example of a high grade glioblastoma to a low grade oligodendroglioma
- The high grade glioma is significantly greater uptake to the surrounding gray and white matter
- Oligodendroglioma has reduced metabolic activity causing the tumor to blend in with the surrounding gray and white matter
- One must conclude that not all tumors have excessive uptake with FDG
- There may be difficulty with high-grade tumor that have been treated with radiation
- Radiation treatment assessment of a brain tumor
- FDG - Uptake that is seen at the edge of the necrotic tissue which may contain viable brain tissue, surviving tumor, or infection (might be a hard call)
- O-(2-[18F]Fluoroethyl0-L-tyrosine (FET) - is amino acid that has a great affinity for tumor cells and is incorporated in areas of high metabolic activity
- FET defines active tumor following a series of radiation treatments

http://jnm.snmjournals.org/content/48/9/1468.full?sid=cc0e620f-fe1c-4127-9abf-4376388456ac
- General (FDG)
- Epilepsy
- Overview
- Complex partial seizures usually occur in the medial temporal lobe (MTL). This significant subgroup of patients are classified with temporal lobe epilepsy (TLE). Often associated with TLE is hippocampus sclerosis (HS)
- If the disorder is unilateral then surgical intervention is suggested by removing 2/3 of the temporal lobe on the affected side. FDG should only be used for seizures in the TML. Seizures beyond the temporal lobe 18F-flumazenil FMZ should be administered
- If the disease is bi-lateral surgery cannot be done because it would leave the patient neurologically impaired
- *PET imaging is a preferred method to determine if a seizures is caused by TLE and also when the patient is in the interictal state
- TLE is positive when there is reduced activity on the affected side. This can extend laterally into the cortex of the temporal lobe
- The key role FDG is to determine if there is uni or bilateral uptake in the MTL which then determines if surgery is warranted. If hypometabolic uptake is noted beyond the TLE no specific conclusion is drawn
- b-Amino-Butyric Acid (GABA) receptors and the use of FMZ
- Is produced to inhibits neurotransmission and reduced excitation that causes epilepsy
- Considered a benzodiazepine receptor (BPR)
- GABAA can be imaged with (11C or18F) FMZ
- When compared to FDG, FMZ only shows up in the presence of GABA. Therefore excessive uptake of FMZ is an indication that the brain is attempting to reduce neurogenic activity to inhibit seizures
- FMZ seems to have applications beyond the temporal foci to include: different types of neocortical focal epilepsy, parietal and occipital lobe epilepsy
- Several articles discuss the use of FMZ to determine partial seizures of the neocortex (2)
- Other tracers
- 11C-carfentanil, 11C-diprenorphine, 18F-cyclofoxy will attach to certain types of opioid receptors in the brain. It is believed that some opioids receptors reduce or limit the area of seizure foci, as in the cast where : opioid receptor show increased uptake with 11C-carfentanil
- Another example11C-deuterium deprenyl shows increased binding to monoamine oxidase, an enzyme found which is found HS tissue
- *Ictal (here is what you need to know)
- PET is generally not useful in this area simply for the fact that it has such a short half-life (when compared to 99mTc)
- Therefore, ECD or HMPAO are the preferred agents since the radiotracer can be injected when the patient goes into a epileptic state (time is the key factor)
- However, PET can be used in the interictal state
- General application of PET is to define MTL in the interical state, but not in the ical state
- Overview
- Dementia
- General comment (two types)
- First type of dementia is directly associated with cognitive behavior, with no other underlining pathology
- Second type of dementia occurs because there is some other underlining pathology (ex. brain tumor or infection)
- *Alzheimer's disease (AD) [3]
- Disease
- This neurological disorder progresses over time and may occur anywhere between the ages of 40 to 90 years
- AD is believed to be an inflammation process, specifically related to beta-protein fragments from the beta-amyloid precursor (glycoprotein). This fragments forms amyloid plaques resulting in neurofibrillary tangles, in turn, this regression slowly causes the brain to atrophy
- Imaging
- FDG-PET is sometimes difficult to image in its earlier stages (~ 66% sensitive). In time, even the false negative patients become positive
- Cortical atrophy starts with decreased uptake in the temporal and parietal lobes and then usually progresses to the frontal lobe. In addition, enlargement of the 3rd/4th ventricles and the choroids-hippocampal fissure are noted
- The earlier you treat the disease with cholinesterase inhibitors the better the patient will respond. Therefore, early intervention is critical
- The above images demonstrate: A - Normal, B - Mild/moderate AD, and C - More advanced AD
- Radiopharmaceuticals
- Florbetapir, Florbetaben, and Flutemetamol all bind to amyloid plaque and appear to be a positive indicated of AD
- However, in a resent article by Chiotis K, et al. (2020) it appears that [18F]THK5317 may even have greater sensitivity in identifying AD as it binds to neurofibrillary tangles, tau protein. When compared to [11C]PIB and 18FDG
- The difference was 95% precision vs 77% precision

http://www.sciencedirect.com/science/article/pii/S2253808915000579

- Disease
- Multi-infarct Dementia (MID)
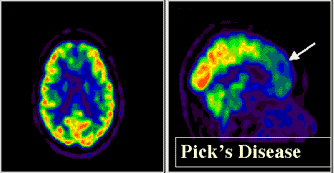
- Frontotemporal Dementia (FTD) - originally referred to as Pick's disease
- Disease
- This neurodegenerative disease causes atrophy of the frontal and temporal lobes
- In Pick disease pick bodies are present in histological analysis
- Imaging
- Looks similar to AD, however, in Pick's hypoperfusion is noted in both frontal and anterior temporal lobes
- Another case of FTD on a 55 year old female with a PET FDG scan - link to article
- CT and MRI may show an abnormal increase in the interhemispheric fissure and enlarged frontal horns

- Disease
- Normal-Pressure Hydrocephalus
- Disease shows normal CSF pressure within dilation of the 3rd/4th ventricles. CSF shunt is used to treat this disease. The patient may be presented with a triad of issues: dementia, urinary incontinence, and ataxia (uncoordinated muscle movement)
- Usually diagnosed with CT or MRI. In PET-FDG reduced perfusion is seen on a global scale and ventricles should appear enlarged
- Alcohol-related dementia
- There is an apparent decrease in uptake in a global scale or at the regional level, sub/cortex or even the left hemisphere
- Reduced uptake has been seen in chronic alcoholics and specifically in the areas of occipital, prefrontal, and cerebella cortices. Furthermore, these areas have been known to contain high level of GABAA receptors
- Creutzfeld-Jakob disease (CDJ)
- Disease caused by a (proteinaceous infectious particles) prion. Spreads quickly through the brain creating a spongiform type tissue. In a very short time the patient goes from dementia to death
- Decreased uptake with PET-FDG is noted, however, actual clinical data is limited
- See example of CDJ on a 56 -year-old female patient was administered with FDG - link to article

- AIDS-related dementia
- HIV involvement in the brain or a result of an opportunistic infection (toxoplasmosis) or AIDS-associated neoplasm
- Approximately 5% of AIDs patients have this related dementia
- PET-FDG shows hypoperfusion in the cerebral cortex
- General comment (two types)
- Extrapyramidal disorders (ED)
- General comments
- These are different types of movement disorders
- Disease cause patients to appear rigid, have nervous tremors, show reduced movement (bradykinesia), bad (degenerative) posture.
- CT and MRI may show disease, however, PET usually picks up the disease(s) at an earlier stage
- *At issue is the regulation of dopamine at the synapse, which transmits an electrical pulse from one neuron to the next (understand the difference between up and down regulation)
- If dopamine is being over produced receptors sites decrease causing "down regulation"
- If dopamine is lacking then the response is to increase the amount of receptors resulting in "up regulation"
- The above chart further illustrates this concept with FDOPA (demonstrates the amount of dopamine production) and RAC (illustrates the amount of D2 receptor sites
- Sometimes there is degeneration of the entire system
RAC Uptake FDOPA Uptake Regulation DOPA Production Receptor Sites Increase Decrease Up Decrease Increase Decrease Increase Down Increase Decrease - Uptake of FDOPA depends on the rate of Dopamine produced
- RAC Uptake relates to the the number of D2 receptors
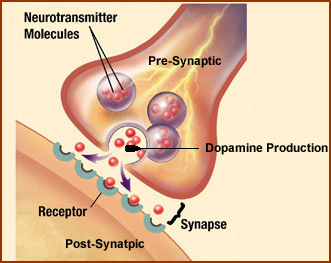
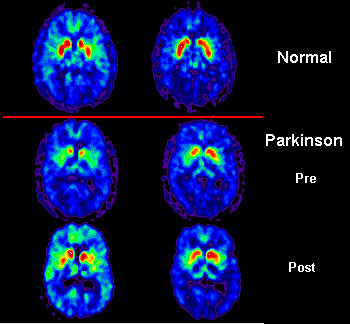
- Parkinson disease (PD)
- Disease
- Nonindustrial projections to the basal ganglia degenerate where there is involvement of the putamen, but not the caudate
- Degeneration occurs at the pre-synaptic side of the dopamine system while the post synaptic remains intact with increased receptor sites. This causes a loss in dopamine production and requires dopamine therapy (supplement)
- Up regulation is noted
- Imaging
- FDG uptake is excessive which may be do to the increased firing of the basal ganglia that is caused by the lack of dopamine. Because of this FDG is not recommended. Why?
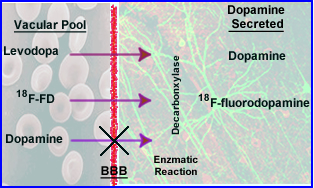
- 18F-fluorodopa (PD) evaluates the dopamine pathway and indication the lack of radiotracer where . Related to dopamine production
- Comment on dopamine production: (1) While FD crosses the BBB, dopamine cannot (because dopamine has a charge preventing it from crossing), (2) However, FD and Levodopa do cross the BBB via enzymatic reaction of decarboxylase, (3) these chemicals converts to "dopamine"
- The above images show uptake of FDOPA in: (1) normal brain, (2) reduced uptake in the putamen, (3) improved uptake to the affected area following dopaminergic therapy
- 11C-raclopride (RAC) evaluates the amount of the amount of D2 receptors and will correlate to an increase in uptake. Most movement disorders, with the exception of PD, show a reduction in D2 receptors
http://www.cerebromente.org.br/n01/pet/pet.htm
- Disease
- Huntington disease (HD)
- Disease
- Genetic issue with significant loss of motor movements occurs over time
- Cognitive issues occur between 30 - 40 years of age with neuron deterioration and gliosis within the striatum
- Microglial activation may play an important role in neuronal death, since excessive amount has been found on autopsy (6)
- Imaging
- Caudate nucleus and putamen show decreased FDG uptake
- The greater the reduction of uptake usually the greater the dementia. Frontal, parietal, and temporal lobes have been effected
- CT and MRI find atrophy, however, this occurs later
- Progressive Supranuclear Palsy (PSP)
- Disease
- PD type symptoms with vertical eye movement that occurs between the ages 60 - 70
- Cell loss is noted in: brainstem, pallidus, and substantia nigra (no complex involvement)
- Midbrain atrophy occurs
- Imaging
- FDG uptake is reduced in the: superior frontal cortex, basal ganglia, thalamus, and pons
- Pre-post synaptic areas are reduced with the putamen being affected
- MRI shows enlargement of ventricles
- Disease
- General comments
- Disease
- Transient ischemic attack (TIA)
- Stenosis within the arterial areas of the brain will causes hemodynamic changes
- Atherosclerotic plaques reduce blood flow. Plaques can break off which may cause a stroke
- Alterations of blood flow (reduced) for whatever reason can lead to more severe issues and must be treated
- How does the brain respond to this reduced perfusion?
- Initially an attempt to increase the extraction fraction of oxygen
- Secondly, dilation of the involved artery(ies)/arterioles
- Over time, as the condition worsens the patient will become symptomatic: loss of vision, alteration in speaking (aphasia), weakness or numbness involving one side of the body
- Stenosis within the arterial areas of the brain will causes hemodynamic changes
- Moyamoya disease (means "something hazy just like a puff of cigarette smoke drifting in the air")
- Abnormal blood flow occurs at the base of the brain
- Stenosis, occlusions, and collateral circulation occurs
- Usually in the areas of the internal carotid arteries
- Depending on age
- Younger patients tend to exhibit TIA type symptoms
- Older patients tend to have intracranial bleeds
- Abnormal blood flow occurs at the base of the brain
- Acute ischemic stroke
- Consequences are usually severe, however, literature indicates that if treated early, re-vascularization may salvage some of the "damaged" area
- Zones of a stroke
- No intervention will help the necrotic tissue caused by perfusion loss
- Surrounding the stroke zone is an area referred to as the penumbra
- If re-vascularization occurs the penumbra tissue may survive (consider the cardiac as another example)
- PET data indicates that tissue with <12 mL/min/100g cannot be salvaged
- PET data that is between 12 to 25 mL/min/100g in the penumbra are salvageable pending re-vascularization and how soon this is done post infarct
- Any tissue that is <65 mL/min/100g and lacks any intervention will eventually become necrotic (time frame - no more than 2 weeks)
- 11C-Flumazenil has been shown to useful to evaluating the penumbra via the uptake of this radiotracer as a candidate for re-vascularization
- Transient ischemic attack (TIA)