Iodine - 131 NP59 Imaging and Physiology
Anatomy and physiology
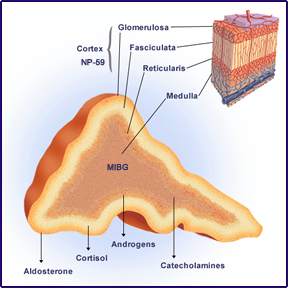
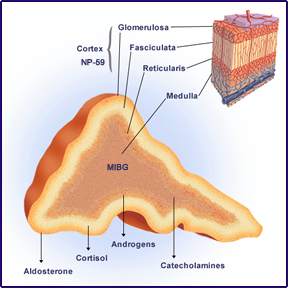
- Adrenal cortex and medulla are composed of different tissues
- Cortex is 90% of the gland by volume with three histological zones
- Zona glomerulosa (outer) - produces aldosterone
- Zona fasciculata (middle) - produces glucocorticoid
- Zona reticularis (inner) - produces mostly androstenedione
- Adrenal medulla secretes catecholamines (refer to MIBG lecture)
|
|
- Generally the right adrenal gland is higher and more posterior and will usually appear slightly hotter in an NMT procedure

- The above diagram demonstrates the negative biofeedback loop associated with the adrenal glands
- Corticotropin Releasing Factor (CRF) or Hormone (CRH) increases it's production
- Stimulates Adrenocorticotropic Hormone (ACTH) production
- Causing Cortisol synthesis
- As cortisol levels increases production CRF and ACTH are reduced
- Ultimately reducing the secretion of cortisol
- Think thyroid and its negative biofeedback loop
- Physiology- adrenal cortex secretes hormones that effect metabolism. This hormones are as follows
- Corticosteroid
- Hydrocorticosteroid (Cortisol) - regulates the use of fats, proteins, and carbohydrates
- Corticosterone - suppresses inflammatory reactions and has an affect on the immune system
- Hydrocoticosteroid and corticosterone work together to suppress the inflammatory process
- Aldosterone - maintains blood volume and pressure and regulates the excretion of sodium in urine
- Androgen (steroids)
- In women this is estrogen
- In man it is testosterone
- Diseases
- Cushing's syndrome
- Body produces excessive amount of cortisol. There are several medications that can contain glucocorticoid which treat inflammation that include: asthma, arthritis,and lupus
- Excessive secretion can be do to high levels of ACTH or CRF production. Just like the thyroid gland responding to excessive levels of TRH and TSH.
- Other individuals that might have high levels of cortisol hormones include: athletes, women in their last trimester, and people suffering from alcoholism, panic disorders, depression, and malnutrition
- Symptoms
- Upper body obesity with thin arms and legs
- Children have slow growth rates and tend to be overweight
- Bones are weak and can result in backaches and/or fractures
- Skin can have purplish pink stretch marks
- High BP and blood sugar
- Person maybe irritable, depressed, or have high levels of anxiety
- Aldosteronism
- Increased levels of aldosterone cause causes the body to retain sodium and lose potassium
- Results in water retention, increased blood volume, and high blood pressure
- Up to 1 in 10 people with high blood pressure may have Aldosteronism
- Radiopharmaceutical
- 131I-6β iodomethyl-19norcholestol - 131I NP-59
- Has great avidity for the adrenal cortex and its uptake is dependent on cholesterol precursor in synthesis of adrenocorticosteroids
- Following injection it is bound to plasma lipoproteins
- High levels of cholesterol in the blood pool reduces the uptake of the radiotracer (how would this effect the scan?)
- Uptake increases with increased levels of ACTH that results in increased production of cortisol
- Uptake of the radiotracer occurs gradually over several days
- Administration of dexamethasone suppresses ACTH production reducing NP-59 uptake
- Adrenal to kidney ratio is usually around 300:1
- Radiation dosimetry (rad/mCi) - this is an issue!
- Adrenal = 25 rad
- Ovaries = 8 rad
- Testes = 2.3 rad
- Total body = 1.2 rad
- Patient Preparation
- Lugol's 1-2 prior and 10-14 post dose
- Dose 1-5 mCi depending on cholesterol level
- Scanning with no suppression
- Start imaging at 4-5 days post dose.
- Should there be increased background levels wait 1-2 more days before imaging
- 131I NP-59 in liver, GB, and colon may interfere with adrenal imaging, but is considered normal uptake
- Laxative 24 hrs prior to imaging is suggested since some of it is secreted by the bowel
- Fatty meal may reduce GB uptake
- Posterior view using a HE collimator is utilized
- Collect counts for for 20 minutes or 50k counts
- Note - if there is no adrenal uptake you will not get 50k counts in 20 minutes
- With a computer % uptake in the adrenals can be calculated. How would you do this?
- Scanning with dexamethasone causes suppresses ACTH secretion
- 4 mg of dexamethasone is given Q4 hrs for 7 days prior to NP-59 dose and 5 days post dose
- DTPA dose prior to imaging may help in adrenal localization
- Normal Adrenal scan
- NP-59 maximum activity occurs at 48 hours post dose, however, since BKG levels are so high imaging cannot be initiated till 4 to 5 days post dose
- 66% of patients have increased activity in the right adrenal when compared to the left
- With suppression normal adrenals are not seen until day 5
- Uptake is .07 to .26%
- Adrenals will image, however, there should be very little uptake
- Images of Cushing Syndrome
 Link
Link
- Cushing - 95% accuracy
- (ACTH dependent)
Bilateral symmetric visualization shows excessive ACTH secretion from within the adrenal, however it can also be seen ectopically. Percent uptake will be 0.3% to as much or greater than 1%. Higher levels of uptake is considered be an ectopic source

- Rare unilateral adrenal hyperplasia
- Asymmetric Visualization of an adrenal is usually hyperplasia. If uptake on one side vs. the other is greater than 50%, it is usually ACTH independent
- Unilateral visualization characteristic of adrenal adenoma. ACTH is suppressed by excessive glucocoritiods secretions and can be up to 0.5 cm in size
- Bilateral Non visualization is Cushing disease with functional adrenocortical carcinoma. Glucocorticoids secretion is in large enough quantities to suppress ACTH and the radiotracer
- Primary Aldosteronism
- Elevated plasma or urine levels of aldosterone
- Images look asymmetrical, but not unilateral
- Does not suppress ACTH production and therefore dexamethasone is useful in identifying disease.

- Hyperplasia - symmetrical uptake before 5 days
- Adenoma - early visualization with little to no uptake in the unaffected adrenal
- Dexamethasone Suppression - suppresses normal adrenal function. Distinguishes from normal to adenoma and bilateral hyperplasia.
- Normal glands are not seen, but may faintly be visualized at the last day (5)
- Known as adrenal gland breakthrough, and not to be considered break dances
- Early unilateral adrenal visualization (< 5 days) suggest adrenal adenoma
- Early bilateral visualization suggest hyperplasia
- This accuracy exceeds 90%
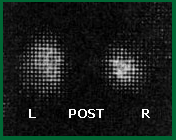
- Unusual case
- This 17 year old female patient was presented with levels of increased: testosterone, dehydroepiandrosterone sulfate (DHEAS), and aldosterone. MRI identified a 9 cm adrenal mass on the right side and the administration of 131I NP-59 visualized the same mass as indicated above. Laparotomy found a adrenocortical carcinoma. This type of tumor is capable of producing a mixture of steroids. Image is noted above.
- This is a very unusual finding. Why?
Return to te Beginning of the Document
Return to the Table of Content
Images and lecture are based from Diagnostic Nuclear Medicine, 3rd edition, Volume 2, Sandler, MP, Patton, JA, et.al., Williams & Wilkins, 1996
Atlas of Iodocholesterol Scintigraphy (NP-59) in Cushing's Syndrome With CT and MR Correlation - Power point presentation can of different disease types can from this article can be found here.
Role of 131I-NP-59 Adrenal Imaging in Patients of ACTH-Independent Cushing’s Syndrome -

 Link
Link