- Tracheobronchial aspiration induced by asthma
- Pulmonary fibrosis
- Hiatal hernia may be a factor which can be combined with either of the other two factors
http://www.nature.com/gimo/contents/pt1/full/gimo30.html
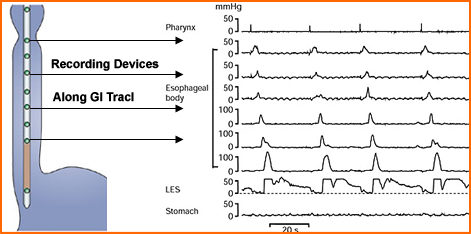
- Esophageal manometry
- In order to diagnose GER this procedure may be used
- Multiple "miniature pressure transducers" identify muscle contraction along the esophagus
- The pressure is then recorded over time as noted in the diagram
- GER would show peristalsis occurring in the opposite direction of normal swallowing
- Oesophageal pH monitoring and the Tuttle Test
(Pediatric Gastroenterology and Clinical Nutrition by Bentley, et al.)
- 0.1 N of HCl is given PO and the patient's pH in the esophagus is monitored
- A drop in the pH level to less than 4 is an indication of GER
- Barium esophagram
- Swallowing barium during a fluoroscopy exam may visualize peristalsis in the esophagus
- Gastroesophageal Reflux Disease: Integrating the Barium Esophagram before and after Antireflux Surgery is an excellent article showing different abnormalities of esophageal diseases. To note: hiatal hernia, obstruction, and GER scarring can be seen
- Barium esophagram and the other above mentioned procedures are not very sensitive in detected GER. Why? Consider the occurrence of reflux and in trying to "catch it"
- General Comment - Following the administration of a radio-liquid drink or meal delayed imaging may identify aspiration of stomach content into the lung
- Consider the time of in which GER will occur and the need to imaging during different time intervals. Does NMT match this need?
- Procedure
- Before bedtime administer 3-5 mCi of 99mTcSC as a beverage
- Follow the radio-liquid administration an additional 30-50 mL of water is given to "wash" down any residue activity
- Imaging before the patient goes to bed is optional, however, imaging thie morning is a requirement
- Camera setup
(PM or AM)
- Collimator - LEHR
- Matrix - 128 or 256
- Aquisition - literature suggest 100k/image, however, if imaging is done immediately following dose administration a higher count density may be considered
- Window - 140 keV at 20%
- Supine imagine - ANT or POST and R-LAT images (exclude as much of the stomach as possible). Why?
- Imaging must be done in the morning and each image usually takes between 20-30 minutes @100k/image
- Results
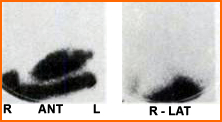
- Case 1 - Following PM radio-liquid administration images were taken the next morning. No activity seen in the lungs, hence no pulmonary aspiration
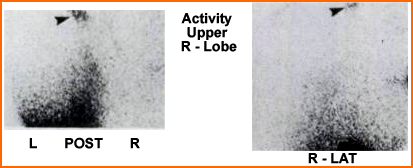
- Case 2 - These AM images indicate aspiration of the radiopharmaceutical into upper right lobe of the lung
- Reasons for missing the aspiration
(think false negative)
- The patient may not GER every night or
- Aspiration may be cleared from the lung before the AM images are taken
- When should this procedure be done?
- Evaluate the effect of or the repair of a hiatal hernia
- Determine the best time to remove an enodtracheal tube
- Determine if asthma has caused an aspiration
- Evaluate the need for a tracheotomy
Information and images on the above information were attained in the following article: Evaluation of Gastro-Pulmonary Aspriation by a Radioactive Technique: Concise Communication. by Reich, et al.
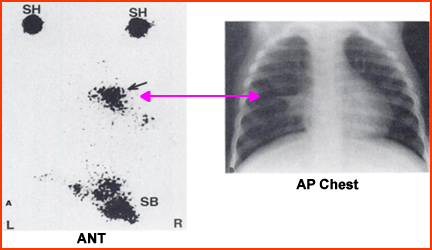
- Another article by Boonyaprapa S, et al. addresses the utilization of pulmonary aspiration exam on the pediatric population. Information and images (below) are a summation of the this article
- Twenty children, for the ages of 1 month to 14 years was evaluated via scintigraphic imaging for possible pulmonary aspiration. Patients selection was based on a prior diagnosis of chronic respiratory infection. Twenty-five percent of these patients showed pulmonary activity there were due to: pneumonitis (3), chronic cough (1), and one TE fistula repair (1)
- Pediatric procedure
(modification to the above approach)
- Dose - 500 :Ci 99mTcSC was mixed in 60 to 100 mL of milk or formula. Older children were given 120 mL of OJ
- Small amount of non-radioactive fluid was given after the radio-liquid
- Five minutes post dose 100k images were taken of the chest/abdomen to include ANT, POST, R/L-LAT projections
- The same Images were repeated 4 hours post dose, as well as the following morning
- 57Co markers where also place on the shoulders to help with anatomical orientation
- Barium esophagram was also administered and positive in 2 of the 20 patients test. Both positive barium studies were positive with nuclear
- The above example is positive for aspiration and was scanned at four hours post administration. This 4 month old female shows activity in the area of the right middle lobe of the lung and corresponds to pneumonitis seen on her chest x-ray
Return to the Beginning of the Document
Return to the Table of Content