- The purpose of this procedure is to evaluate lacrimal drainage.
- Usually the procedure is done if the patient has epiphora (water eye(s))
- Epiphora maybe due to excessive tear production or blockage in a tear duct that prevents drainage
- Perhaps the procedure of choice would be a dacryocystogram (radiology), however, this exam is a lot more invasive that its counterpart, nuclear medicine
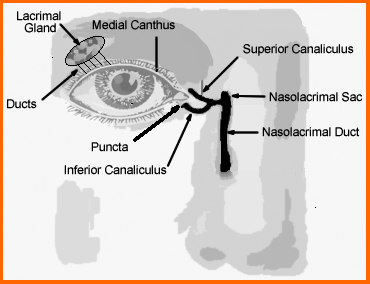
- The anatomy of tear production and drainage must be reviewed
- Tears flow as follows
- Tears flow from the lacrimal gland down small ducts that bath the eyeball
- Tears flow towards the medial position of the eye as it passes the medial canthus
- Then the liquid enters opening known as the puncta
- Tears continue down the medial and inferior canaliculi to the nasolacrimal sac and duct
- The nasolacrimal duct then drains into the sinus
- A blockage can occur anywhere along the nasolacrimal duct system
- Diseases that cause obstruction
- Epiphora - watery eye
- Periocular - occurs around the eye
- Causes
- Congenital
- Blockage do to stone or tumor
- Infection
- Procedure
- Dose preparation
- Dose is between 100 to 200 μCi per eye
- To achieve correct activity you need to remember that 20 drops is about equal to 1 mL
- Therefore, if you take 200 μCi and multiple by 20 drops (see conversion calculator) you get a concentration of 4.0 mCi
- Hence a diluted vial of 99mTcO4- must have a concentration of 4.0 mCi/mL
- In the above example a 10 mL solution is calculated
- Place the solution into a small bottle that contains an eyedropper. The entire container should be placed it need a lead container until needed
- In the hotlab I decided to see how accurate a 200μCi dose so I prepared a 4.0 mCi/mL solution and came up with the above result. It appears that my μCi per drop is a little off?

- Camera/patient setup
- Pinhole collimator
- Matrix at 64 or 128
- Acquire 30 seconds per frame for 5 minutes
- Place the patient in a supine position and immobilize the head
- The field of view should be set to acquire both eyes yet bring the detector in, as close as possible. Remember with a pinhole the further away the collimator is the smaller the area of interest
- To assure that both eyes are in then FOV use a hot marker
- Acquisition
- Set the patient up before placing the drops in the eye
- Put one drop into the lateral ends of each canthus
- Start imaging
- Normal tear flow, the activity should appear in the nasolacrimal sac and duct within several minutes
- Non-filling of the sac or duct is an indication of blockage
- Optional maneuvers - If the flow of activity seems "sluggish"
- Digital massage over the nasolacrimal sac and duct, which may facilitate movement within the duct.
- Additional drops of saline may assist in flushing the radiopharmaceutical to into the puncta
- If the activity shows little movement, wash the eye out saline and a sponge. This may help to determine if there is a blockage
- Evaluation of the scan - Compare both eyes by observing the flow
- Normal shows drainage through the system in a matter of several minutes
- Partial blockage is seen if one side drains slower than the other
- Complete blockage is indicated when the activity does not move at all
- Dacryocystography vs. dacryoscintigraphy
- The radiology procedure
- Requires cannulation and injection of contrast into the puncta. This is usually painful procedure and may traumatize the eye as the contrast is injected into a blocked nasolacrimal duct
- It does give excellent anatomical detail and is considered a simple procedure
- Nuclear medicine
- Is recommended as the initial step to determine if there is a problem
- There is no trauma or pain in this procedure and it analyzes tear flow from a physiologic standpoint
- Unfortunately its anatomical detail is limited
- This procedure might be considered for pre and post surgery to determine if blockage has been removed
- Case presentation - Normal



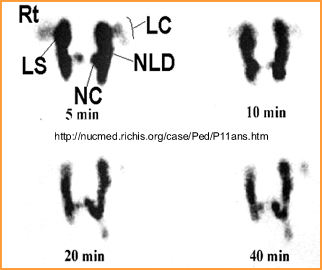
- This procedure shows normal flow of salivary tears
- Compare this above image to the drawing seen at the beginning of the lecture
Abnormal Case I
- Blockage is very pronounced
- Blockage is greater on the left than it is on the right
- At 40 minutes the radiotracer does not go pass the proximal end of the nasolacrimal sac (left or right)
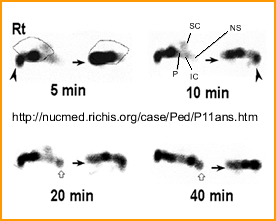
- The image on the left shows normal tear flow with generalized anatomy being identified
- The image on the right is abnormal with a blockage noted in the nasolacrimal duct
- Homework
- Comparative Study on Dacryoscintigraphy and Contrast Dacryocystography
- Dacryoscintigraphy: A Pictorial Essay
Abnormal Case II
Reading assignments:
Return to the Beginning of the Page
Return to the Table of Content
9/23
Lecture material and images were taken from: Nuclear Medicine Diagnosis and Therapy, Harbert, JC, Eckel man, WC, and Neumann, RD.Thieme Medical Publishers, Inc., NY,NY 1996